Newsletter Signup - Under Article / In Page
"*" indicates required fields
By Michael Pisano, executive vice president, proteomics, Discovery Life Sciences
In oncology, characterizing genetic markers is a powerful tool, but it only tells part of the story. A burgeoning field called proteogenomics is helping uncover downstream biomarkers that represent the functional changes resulting from gene expression that will launch research and development of new, targeted cancer therapies forward.
Cancer biomarkers can reveal the nuances of a patient’s disease and indicate which targeted therapies might be most effective. In recent decades, the field of genomics has made great strides in identifying gene mutations that serve as markers for specific cancer types. However, a genetic mutation might not inform scientists about how that mutated gene impacts a cell’s physiology. Proteogenomics can provide clarity to the function of the genome by providing information about downstream effects of genetic mutations, enabling scientists to accelerate the development of new, targeted cancer therapies.
Proteogenomics and the discovery of biomarkers for cancer research
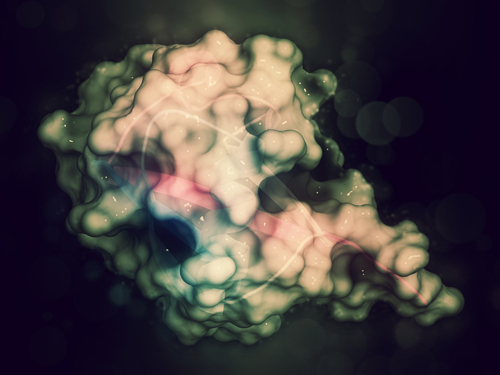
Proteogenomics paints a detailed picture of how gene expression manifests in a cell by looking beyond genome information and exploring the roles proteins are playing in the biology being studied. For example, a single gene mutation has the potential to affect numerous cellular pathways, of which any one presents multiple proteins as putative therapeutic targets.
Furthermore, these proteins can also serve as biomarkers. In cancer, neoantigens form on cancer cells due to a mutated gene. Their presence could be a marker that defines the malignancy. Additionally, if peptides from the neoantigen present on the major histocompatibility complex (MHC) molecules, it may also be used for immunotherapy purposes as the basis of peptide vaccines against the cancer.
Can personalized medicine make the drug development process more efficient?
Everyone is unique in their response to therapeutic intervention. Individuals might experience different side effects, varying treatment efficacies, and specific toxicity issues. Every patient will benefit from personalized treatment tuned to their specific disease and biological makeup. Biomarker discovery and validation must start early in the drug discovery process, selecting those that show the strongest correlation with disease state and/or treatment response. Biomarkers are key to personalized medicine and can certainly improve the success rate of the drug development process.
One area in which biomarkers support the drug development process is by utilization in clinical trials. Screening potential trial participants during enrollment helps recruit and select a target population most likely to benefit from the treatment, therefore maximizing the chances of running a successful trial.
Biomarkers as companion diagnostics are also used for highly targeted therapies optimizing treatment regimens for individuals. Subsequently, when a therapy comes to market, doctors can evaluate patients’ biomarker profiles and use that information to prescribe treatment accordingly.
Although discovering biomarkers with proteogenomics is no simple task, those in the biopharma community have recognized that they will be vital to moving the field forward and will ultimately expand what is possible through personalized medicine.
Biomarkers in cancer research: an untapped potential
The discovery of new DNA and RNA biomarkers is proceeding rapidly thanks to inexpensive, high-throughput technologies. However, protein and lipid biomarkers have lagged.
While proteins are readily used as clinical markers in diagnostic kits and other clinical lab tests, discovering new protein biomarkers to aid in clinical trials is more challenging. Proteomics has lagged genomics and transcriptomics because, until very recently, the technologies and experiments for studying large sets of samples were simply too low throughput, low capacity, and expensive. However, newer technology platforms have been developed and are in practice that enable higher throughput proteomic studies that are scalable. These platforms should enable proteomics to be utilized in large scale population studies and clinical trials.
On the other hand, the field of lipidomics is in its infancy. Lipidomics is a specialized component of metabolomics that focuses on lipids which are medium-sized molecules as opposed to small-molecule metabolites. While lipidomics has great potential to expand our understanding of cancer physiology, mass spectrometry-based lipid databases are still relatively deficient. With additional research, lipidomics will likely become a major part of multi-omic studies in research and drug development. While biomarker research of proteins and lipids is still gaining steam, both fields promise to expand on the information that can be gleaned from DNA and RNA, ultimately accelerating drug development programs and advancing precision medicine.
Proteogenomic advancement to expand the biomarker repertoire
Technology is a major driving force behind drug and biomarker discovery and development.
Scalability, throughput, and affordability all accelerate research. Technologies to query protein species are beginning to offer data on a scale that will make protein-based biomarker discovery significantly more efficient. Targeted immune-based assays can measure about 7,000 proteins.
Likewise, using a high throughput method, untargeted assays based on mass spectrometry can identify ~20,000. And, while low-throughput, breakthroughs in single-cell technology provide insight into proteins’ roles at the single cell type level, providing researchers with a new kind of data previously not readily available.
As companies develop better, faster, cheaper sample preparation approaches, instruments, and chemistries to run assays, every piece of that workflow must keep up with the others for proteogenomic advancement to continue unhindered. Simultaneously, focus cannot be lost that the whole is greater than the sum of its parts. Integrating data from platforms designed to analyze multiple cellular phenomena (multi-omics or systems biology) is paramount. Like a puzzle, looking at a single piece of data will not reveal the whole picture because it lacks context. But by putting the puzzle pieces together, the whole image suddenly becomes clear.
Computation advances will provide context
How does one bring together disparate data sets and information to illuminate the pathways being affected by a genetic mutation? Computational biology, bioinformatics, and AI can help researchers search for downstream biomarkers by giving context to the data from gene expression, epigenetics, protein expression, protein interactions, and metabolic profiles. However, the task is monumentally complicated, and the field is still working out how best to process it.
Leaders in the field, such as the National Cancer Institute’s Clinical Proteomic Tumor Analysis Consortium (CPTAC) at the National Institutes of Health, are working to define how to proceed.
However, much information about the underlying biology still needs to be discovered. For example, protein-protein interaction maps look chaotic now, with every protein interacting with countless others. What is the significance of each interaction? To synthesize this complex information, we need to build training sets that will enable us to reconstruct these biological pathways—and build software that can do this routinely.
While much work remains to decide which computational approaches will best serve proteogenomics, every new advancement may accelerate the discovery of new cancer biomarkers and their use in clinical research.
How to accelerate biomarker discovery
In clinical research, timing is critical. As mentioned above, biomarker discovery and validation must start early in the drug discovery process. Drug development programs must establish what specific biomarkers will be used to enroll patients before initiating a clinical trial.
Establishing these biomarkers requires studies that may take several years to complete. However, by partnering with a company that can aid in the biomarker discovery and development process, the program can advance more efficiently, particularly if that partnering company provides a one-stop shop where scientists can do all the studies within the same organization.
An ideal partner should have extensive multi-omics capabilities.
While drug development programs may prefer to provide their own samples for analytical testing, having a partner that could also provide fully characterized (sequenced with proteomic profiles) biospecimens or samples is a plus. Having available matched tissue and biofluids from the patients is like gold for biomarker discovery programs.
Through carefully designed proteogenomic studies, drug development programs can tease out vital information about disease mechanism and mechanism of action of drugs and identify putative drug targets, and biomarkers. Each piece of information brings us one step closer to understanding how diseases like cancer manifests in each individual and how best to treat their “unique” disease.
Oncology R&D trends and breakthrough innovations