As the Covid-19 pandemic sweeps the world, cancer research is proving a valuable resource for developing new treatments for infectious diseases by harnessing the power of the immune system.
Despite the growing number of viral outbreaks of different sizes and severity we have observed in the past years, the infectious disease market is far behind the oncology one, which is often seen as more profitable. Within the cancer market, immuno-oncology has been in the center of attention for the past decade. Research in this field has delivered impressive achievements in understanding the interactions between the tumor and the host immune system that have resulted in new treatments, such as checkpoint inhibitors and CAR T-cell therapies, which benefit some cancer patients that previously had few options left.
Fortunately, these advancements in immuno-oncology can be used in the fight against infectious diseases. We are currently observing the repurposing of immuno-oncology drugs and technologies in response to the global health emergency of Covid-19.
Enhancing existing vaccines
Immune T cells have the natural ability to identify tumor antigens and attack cancer cells. Thus, harnessing the power of T cells is emerging as a leading strategy in immuno-oncology research, and scientists are leveraging ways to amplify and direct this part of the immune system against Covid-19.
“Our T cell response has evolved to fight viruses, not cancer. When we use the T cell response to fight cancer, we try to adopt an antiviral response to cancer,” explained Vincenzo Cerullo, scientific founder of Valo Therapeutics and professor at the University of Helsinki. “During Covid-19, what we realized is that we are going back to what nature has done, which is fighting the virus with a T cell response.”
Valo Therapeutics is creating cancer vaccines that induce a response from T cells. These vaccines consist of presenting cancer antigens to the T cells by putting them on the surface of a modified virus. This way the T cells learn to identify and attack cancer cells as if they were a viral threat.
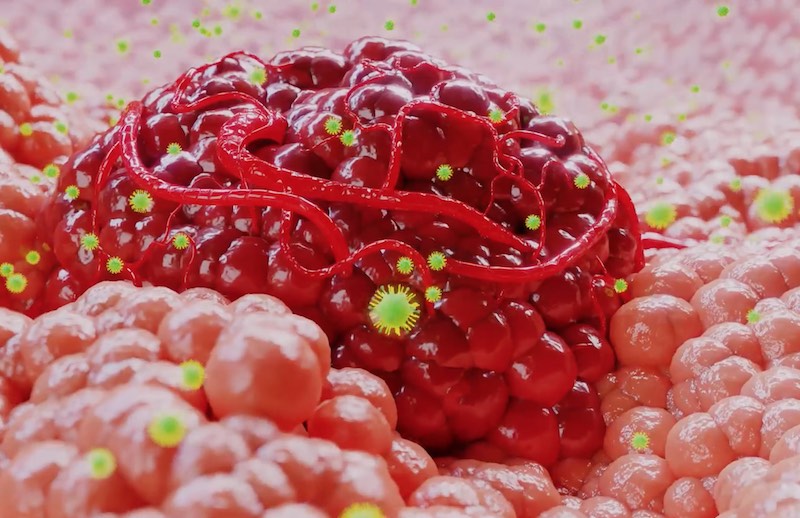
The company is now applying this technology to Covid-19 vaccine development and has identified multiple viral antigens to create a vaccine. Its strategy is to link these viral antigens to an already existing vaccine for a similar virus, which will accelerate the transition to clinical development. If successful, it would be a rapidly available, multitarget, enhanced Covid-19 vaccine.
“We had never thought that this technology would be useful for infectious diseases,” said Cerullo. “Pathogens, they change a lot, but they don’t change as much as cancer. (…) I never thought that this urgency would be important in infectious diseases until we dealt with Covid-19. In that sense, our biggest features, rapidity and adaptability, that we thought were useless for infectious disease, after Covid-19 we thought that they are very useful because, in a matter of weeks, we can have an enhanced vaccine.”
Targeting all coronavirus strains
The French biotech OSE Immunotherapeutics is developing immunotherapies for oncology and autoimmune diseases. One of its technologies consists of screening and identifying the cancer antigens that are most likely to induce a robust T cell response. An extra mutation is added to the antigens to further increase the immune response against them.
OSE aims to generate a prophylactic vaccine covering all coronaviruses. The vaccine is intended to protect against Covid-19 as well as any possible future outbreaks of other strains from the coronavirus family.
The company’s strategy reflects a lesson learned from oncology. “We are designing our vaccine based on the evolution of tumors,” says Nicolas Poirier, Chief Scientific Officer at OSE Immunotherapeutics. He explained that the company takes into account the variability seen across patients in the case of cancer, and across viral strains in the case of coronavirus, to select the antigens that are most common and therefore are less likely to mutate or evolve.
The scientific team of OSE has analyzed more than 7,000 different strains of coronavirus and has identified antigens that the virus behind Covid-19 shares with those that caused the SARS and MERS outbreaks in 2003 and 2012, respectively. “We mutated [these antigens] as we perform in cancers to generate a new vaccine that will focus on generating T cells that can migrate in the lung, reside in the lung, and wait for the virus,” said Poirier. “As soon as the virus enters, the T cells will be there and will eliminate the infected cells and block the replication of the virus.”
Quenching inflammation
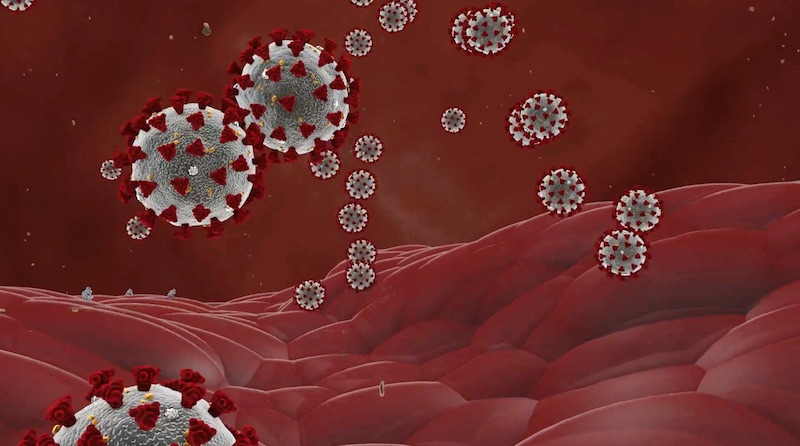
One approach in cancer immunotherapy is to limit the local inflammation that the tumor causes, which plays an integral part in its growth, resistance, and metastasis to other parts of the body. Similarly, an overactivation of the immune system causing local inflammation in the lungs is a significant source of complications in Covid-19 patients. Reducing the number of deaths related to these complications is a crucial step in the fight against the pandemic.
These life-threatening overactivations are governed by the innate arm of the immune system. This is the main focus of French biotech Innate Pharma, which develops cancer treatments targeting the innate immune system.
Innate Pharma is repurposing one of its experimental cancer drugs to treat the most severe cases of Covid-19, where the immune system overreacts. The drug, called Avdoralimab, is an antibody that blocks the receptor of C5a, an inflammatory protein produced by some cells of the innate immune system.
A study run in cooperation with two French hospitals revealed that the C5a protein was found in higher amounts in severe cases of Covid-19 with pneumonia or acute respiratory distress syndrome. “We could see that the level of circulating C5a is commensurate to the severity of the disease,” explains Eric Vivier, Chief Scientific Officer of Innate Pharma and professor at the Aix-Marseille University. “By blocking this pathway using Avdoralimab, we expect to induce a better control over inflammation in Covid-19 patients.”
Like Cerullo, Vivier sees the ongoing repurposing of cancer drugs for infectious diseases as a way of returning to the roots. “The understanding of the immune response was based on its dissection against microbes. That led to the immuno-oncology field, and that led to the development of molecules that can act on the immune response. So now, some of these molecules can be repositioned, repurposed in the field of inflammation, and, in particular, in the field of Covid-19.”
The actions of these companies in response to the pandemic have brought up the critical reminder that the immune system underlies every pathological condition, and that the advancements made in the past years are not restricted to the oncology field. “Immunology rather than immuno-oncology will be basically re-evaluated as an important part of all of our research,” reflects Cerullo.
The ongoing events are also giving us ground to reflect on how interconnected scientific progress is. It is impressive to observe how advancements in one field are contributing to more neglected areas, and how quickly actions were taken in this direction. “Many big companies and biotechs were very creative on how they can accelerate their process,” points out Poirier.
All this leaves us with the hope that the trends that are reshaping the way science is appreciated, conducted, and shared will remain after the crisis has passed.
Cover illustration by Elena Resko, images via Valo Therapeutics and Innate Pharma





