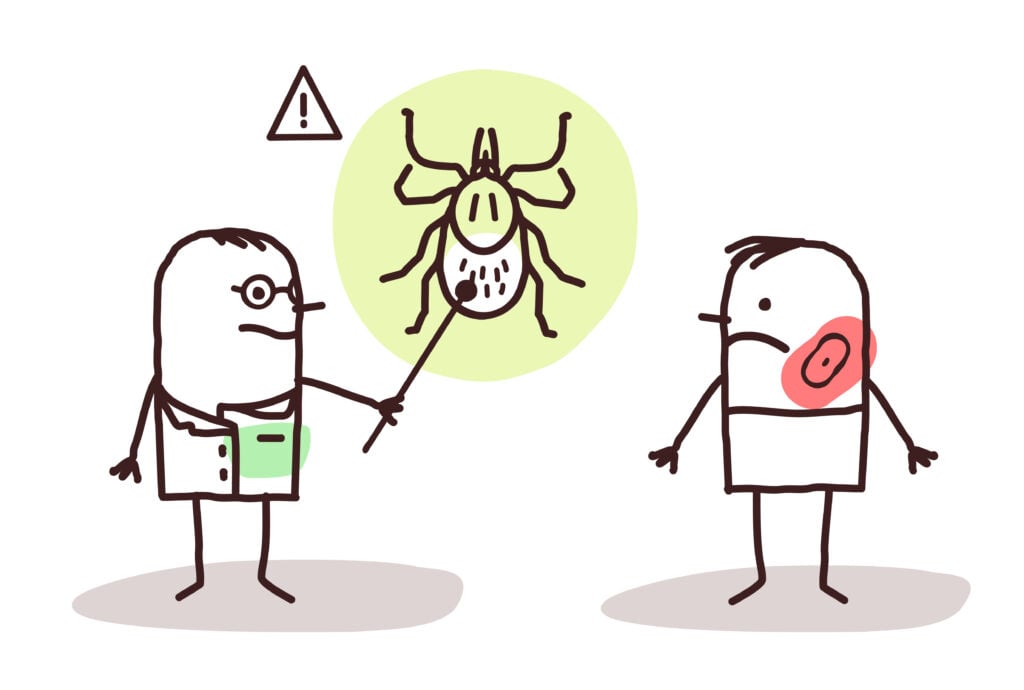
Lyme disease is the most common vector-borne disease in the U.S. – a new CDC estimate suggests that approximately 476,000 Americans are diagnosed with Lyme disease each year – and it is caused by the bacterium Borrelia burgdorferi. It is primarily transmitted to humans through the bite of an infected Ixodes tick; also known as a black-legged tick or a deer tick.
Although transmission does not occur instantaneously when a tick bites someone – in fact, it must be attached to an individual for 36 to 48 hours or longer to transmit the disease – it can often take a long time for someone to notice that the tick is attached to them, with some not even noticing at all until it unknowingly drops off.
This is due to the fact that ticks are small, especially nymphs, which are young ticks in between the larval and adult stage, and pose the highest risk of passing on Lyme disease. These are approximately the size of a poppy seed and are extremely abundant.
If someone does contract the disease, a common early indication is the ‘bull’s eye’ rash that usually develops near the location of the tick bite. As the rash increases in size, it clears in the middle and develops a red ring around the outside. Other early symptoms can also include fever, headache, fatigue and joint stiffness.
These symptoms could lead to someone seeking out a test, and, if it comes back positive, treatment with antibiotics for two to four weeks usually follows. For many people, this is enough to clear the infection; but it doesn’t work for everyone and some people continue to experience symptoms.
“We don’t know whether symptoms are due to active infection still, nerve damage or some sort of auto-immune reaction. There is no test at the moment that can determine this. This is similar to long COVID – no-one really knows the cause or what to do about it.”
What is chronic Lyme disease?
Despite treatment working for most people, in around 10 to 20% of people who are treated with the recommended dose of antibiotics, the symptoms of Lyme disease will persist, even after they have completed treatment. This is known as post-treatment Lyme disease, and the symptoms, such as fatigue, joint or muscle aches and cognitive dysfunction, may last up to six months or longer.
It is unknown why some people develop post-treatment Lyme disease. “We don’t know whether symptoms are due to active infection still, nerve damage or some sort of auto-immune reaction. There is no test at the moment that can determine this. This is similar to long COVID – no-one really knows the cause or what to do about it,” explained Stella Huyshe-Shires, chair of Lyme Disease Action.
Moreover, an unknown number of people who contract the disease remain undiagnosed and untreated for years, or even a lifetime. When this happens, the disease is allowed to spread, potentially reaching the joints, heart and central nervous system (CNS), and can result in severe and debilitating symptoms, such as arthritis, facial weakness and paralysis – known as Bell’s palsy – and numbness and pain in the arms and legs.
How new Lyme disease tests could help to prevent chronic infection
When it comes to Lyme disease, an early diagnosis is crucial, because the sooner someone is treated with antibiotics, the less likely they are to develop persistent symptoms.
However, due to the fact that people might not notice they have been bitten by a tick, and because Lyme disease symptoms can be similar to other conditions, the disease can be quite challenging to diagnose.
Furthermore, if someone does get tested, currently available tests could potentially miss the infection.
The main type of test for Lyme disease at the moment is a blood test that looks for antibodies to the Lyme disease bacteria, which follows a two-tier system.
Tier one involves a conventional enzyme-linked immunoassay (ELISA) test, and if the result is borderline or positive, the sample is sent to a specialist reference laboratory for further testing. The tier two test is then an immunoblot – or Western blot – which confirms Lyme disease and also helps to identify a false positive tier one result.
But if antibodies have not developed sufficiently – it could take a few weeks for the body to make enough antibodies to show a positive result – the test could show up as negative despite someone having an active Lyme disease infection.
Equally, the presence of antibodies may not indicate active infection. “Once someone has developed the antibodies on which the current test relies, those antibodies may stay for years, despite the person being cured. So that person will still test positive. You can get Lyme disease more than once, and this makes it difficult to use the current tests to determine: ‘is this Lyme disease?’” said Huyshe-Shires.
And, according to Mollie Jewett, associate professor and head of the Immunity and Pathogenesis Division at Burnett School of Biomedical Sciences, UCF College of Medicine in the U.S., another issue with current tests is that they may not be standardized across diagnostic laboratories, plus expertise is required for accurate interpretation of the results, and they are somewhat subjective.
Therefore, developing a new, standardized active test that can directly detect the Lyme disease bacteria, rather than just antibodies to the bacteria, could greatly improve testing accuracy, and it could allow people to be diagnosed much earlier. This means less people will go undiagnosed and can potentially receive treatment at an earlier stage, making it much more likely that their symptoms will not become chronic.
Challenges of creating a more effective test for Lyme disease
It is all well and good saying that a new test for Lyme disease is needed, but actually developing one is quite a difficult task. As Huyshe-Shires pointed out, creating a test that detects active disease probably depends on very new technology to find biomarkers, and this is something that will not happen overnight.
Additionally, Jewett explained that developing an active test is so challenging due to the transient window of time in which the Lyme disease bacteria is present at detectable levels in the blood.
“The biology of B. burgdorferi is such that the bacteria does not thrive in the blood. It is only transiently in the blood in the first seven to 14 days after infection. After this time the bacteria has spread to other places in the body such as the joints, the heart and the nervous system. These are the sites of infection that are characteristic of Lyme disease,” she said.
“The direct diagnostic test of Lyme disease, therefore, has to be highly sensitive to be able to detect the bacteria even when it is only present in small amounts in the blood. I like to use the analogy of fishing – the best diagnostic test for direct detection of B. burgdorferi requires having many hooks in the water (sensitivity) and the optimum bait to capture what you are fishing for (specificity). It is also very important that anyone can be a successful fisherman (the diagnostic test must be objective and straightforward to interpret).”
Active test for Lyme disease
Despite the challenges, researchers are working on coming up with new Lyme disease tests that detect active infection, and are rapid and more accurate.
For example, Jewett is involved in developing a rapid test that can detect the disease weeks earlier than current tests, which would overcome the “diagnostic blind spot” that occurs prior to at least 14 days after infection – in which there are not enough antibodies for current tests to pick up the infection. It would also eliminate the need to visit diagnostic labs and wait for results.
“The test that we are developing to directly detect B. burgdorferi has the potential to overcome this “diagnostic blind spot” allowing people to be definitely diagnosed with Lyme disease earlier, and therefore, allowing them to receive appropriate treatment sooner,” explained Jewett.
“In addition to directly detecting B. burgdorferi with our test, our team is developing a point-of-care diagnostic device that can be used in the doctor’s office to run the test and provide the results of the diagnostic test in as little as 15 minutes. Current test must be sent out to a diagnostic company and the results are not available for multiple days.”
Other types of new Lyme disease tests
There could also be new tests that, even though they do not necessarily detect active infection, are still more accurate than the tests we currently have available.
One such example is a testing mechanism that was identified by researchers at Tufts University School of Medicine, which detects antibodies that infected individuals produce against a substance the Lyme disease bacteria acquires from the host in order to grow, known as autoantibodies – antibodies that mistakenly target and react with a person’s tissues or organs.
Researchers believe that tests to detect these could offer a way to diagnose Lyme disease sooner, know whether treatment with antibiotics is working, and identify people who have been re-infected.
In addition, biotech company EpitogenX is working to adapt COVID-19 testing technology in order to create a better Lyme disease test.
Dr Abdo Alnabulsi, chief executive officer (CEO) of EpitogenX, stated: “We are working on a serology based antibody test for the detection of Lyme disease. The test will be developed using our proprietary technology ‘EpitoGen’, a multiplexing biological system whereby multiple biomarker targets can be assembled into one chimeric antigen. We will also employ use of our in-house AI system to identify antigenic regions within the Lyme’s pathogen.”
“The ability of our technology to display multiple biomarker targets means the test will be extremely sensitive and specific to Lyme. The test will be available as lab-based (ELISA) and as point-of-care lateral flow versions.”
Alnabulsi also added that both versions of the test will be easy to use and cheaper than existing platforms, allowing them to be adopted worldwide.
New treatments on the horizon for Lyme disease
Of course, the surest way of preventing chronic Lyme disease is to have a treatment that can prevent or cure a Lyme disease infection.
Fortunately, there could be a new treatment on the horizon in the form of a vaccine, with Valneva and Pfizer’s VLA15 vaccine currently in advanced stage clinical development.
VLA 15 is a multivalent recombinant protein vaccine that targets the outer surface protein A of B. burgdorferi. It targets six serotypes of Borrelia that represent the most common pathogenic strains found in the U.S. and Europe.
The vaccine is currently being tested in a phase 3 study, called VALOR, to assess its efficacy, safety, tolerability, and immunogenicity in participants five years and older.
The study was initiated in August 2022, and is taking place over 29 months. During the first year, as part of the primary series, participants will receive three doses of VLA15. They will then receive one booster dose approximately one year after completion of the primary immunization.
The vaccine received a fast track designation from the U.S. Food and Drug Administration (FDA) in 2017, and Pfizer could potentially submit a Biologics License Application (BLA) to the FDA, and Marketing Authorization Application (MAA) to the European Medicines Agency (EMA) in 2025, pending successful completion of the VALOR study.
If the vaccine were to be approved for use, along with new rapid Lyme disease tests, it could be a groundbreaking step in preventing people from developing chronic Lyme disease.

New technologies related to Lyme disease tests
- Early Lyme Disease Detection – Colorado State University Differentiation of Early Lyme Disease from Southern Tick-Associated Rash Illness (STARI) – Colorado State University
- A Rapid, High Content, Reagent Sparing, Fluorescent Plasmonic Assay Platform for Multiplexed Serum Antibody Detection in Lyme Disease and COVID-19 – SUNY Research Foundation