Bath, in South West England, has a lot more besides its historic beauty…The Jenkins Chemistry lab at the University of Bath has a fair few innovative solutions to the problem of infectious disease detection. Their latest design is a burns dressing which glows when a pathogenic biofilm is detected (as part of the Bacteriosafe Project) which collectively has up to €5.12M funding from the European Commission’s FP7 Program.
 The Jenkins lab at the University has several focal areas based on limiting the spread of infectious diseases. From looking at materials used in developing med-tech (i.e. anti-biofilm polymers for catheters etc.) to identification of such hospital-acquired pathogens (using the IO system), Jenkins and his team have been comprehensive in their approach to anti-microbial innovation.
The Jenkins lab at the University has several focal areas based on limiting the spread of infectious diseases. From looking at materials used in developing med-tech (i.e. anti-biofilm polymers for catheters etc.) to identification of such hospital-acquired pathogens (using the IO system), Jenkins and his team have been comprehensive in their approach to anti-microbial innovation.
Infection resulting from wound dressings is also a major problem in burns victims. However, the biggest problem lies in the detection of these pathogens, which the team has now addressed with a ‘smart’ coated dressing in collaboration with The South West UK Children’s Burn Centre in Bristol and the Blond McIndoe Research Foundation (Sussex).
On contact with pathogenic bacterial toxins, nano micro-capsules which are grafted into the dressing are lysed, releasing antibiotics which kill the bacteria. Since lysis of these capsules also changes the dressing colour, the system works as a pathogen-specific indicator as to when a burn needs more medical attention. This, therefore, avoids unnecessary use of antibiotics (for treatment of burns where only non-pathogenic strains of E. coli are present).
Published in the ACS Applied Materials & Interfaces, Jenkins and his team admit there is a long way to go yet, with tolerability and safety testing of their prototype projected to be completed by 2017.
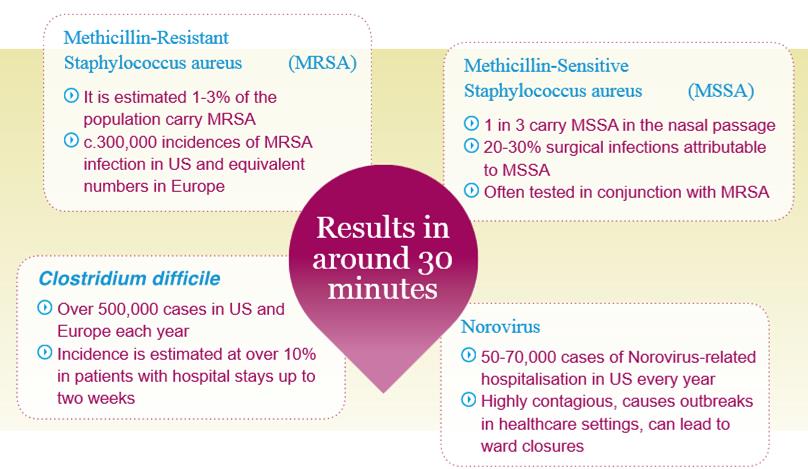
Meanwhile, Atlas Genetics is a biotech spin-off from the University, which in conjunction with the Jenkins lab has developed the IO cartridge system for use in detection of pathogens in hospitals. The test utilises an “on-chip PCR amplification of target gene sequences coupled with electrochemical detection“.
Other biotechs are competing to develop a similar cartridge based diagnosis kit, including the Alena System (from Canadian Axela, and tested in the EU by Hutman Diagnostics) and the Unyvero System (from German Curetis). Despite this, Atlas Genetics has strong financial backing with investors like Novartis Venture Funds and Johnson & Johnson backing the IO system.
This latest addition to the University’s anti-microbial arsenal is really exciting (not to mention eye-catching), and could really help prevent the over-prescription of antibiotics.





