Vertex Pharmaceuticals (Europe) and CRISPR Therapeutics have announced that the European Medicines Agency (EMA) has validated the Marketing Authorization Application of exa-cel for the treatment of sickle cell disease (SCD) and transfusion-dependent beta thalassemia (TDT).
The submission is supported by two global phase 3 studies investigating exa-cel as a potential one-time therapy for people with SCD or TDT.
“Today marks a significant milestone in our efforts to bring a new one-time therapy to people living with sickle cell disease or transfusion-dependent beta thalassemia,” said Nia Tatsis, executive vice president, chief regulatory and quality officer.
“We look forward to working with the EMA on our application, the first for a CRISPR-based therapy for a genetic disease.”
Exa-cel has been granted Orphan Drug Designation from the European Commission, as well as Priority Medicines (PRIME) designation for both SCD and TDT from the EMA. Vertex has also begun the rolling Biologics License Application (BLA) submission to the U.S. Food and Drug Administration and expects to complete the BLA by the end of the first quarter.
About exagamglogene autotemcel (exa-cel)
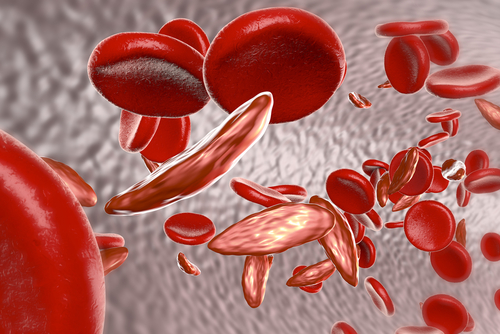
Exa-cel, formerly known as CTX001, is an investigational, autologous, ex vivo CRISPR/Cas9 gene-edited therapy being evaluated for patients with SCD or TDT, in which a patient’s own hematopoietic stem cells are edited to produce high levels of fetal hemoglobin (HbF; hemoglobin F) in red blood cells.
HbF is the form of the oxygen-carrying hemoglobin that is naturally present during fetal development, which then switches to the adult form of hemoglobin after birth. The elevation of HbF by exa-cel has the potential to reduce or eliminate painful and debilitating vaso-occlusive crises for patients with SCD and alleviate transfusion requirements for patients with TDT. Earlier results from these ongoing trials were published in The New England Journal of Medicine in January of 2021 and presented at the European Hematology Association Congress in June 2022.
Gene-editing process
Patients have their own hematopoietic stem and progenitor cells collected from peripheral blood. The patient’s cells are then edited using CRISPR/Cas9 technology. The edited cells, exa-cel, are then infused back into the patient as part of an autologous hematopoietic stem cell transplant (HSCT), a process involving a patient being treated with myeloablative busulfan conditioning. Patients undergoing HSCT may also encounter side effects (ranging from mild to severe) that are unrelated to the administration of exa-cel.
Patients are initially monitored to determine when the edited cells begin to produce mature blood cells, a process known as engraftment. After engraftment, patients will continue to be monitored to track the impact of exa-cel on multiple measures of disease and for safety.
Vertex/CRISPR collaboration
Vertex and CRISPR Therapeutics entered into a strategic research collaboration in 2015, to focus on the use of CRISPR/Cas9 to discover and develop potential new treatments aimed at the underlying genetic causes of human disease. Exa-cel represents the first potential treatment to emerge from the joint research program. Under an amended collaboration agreement, Vertex now leads global development, manufacturing and commercialization of exa-cel and splits program costs and profits worldwide 60/40 with CRISPR Therapeutics.
Partnering 2030: The Biotech Perspective 2023