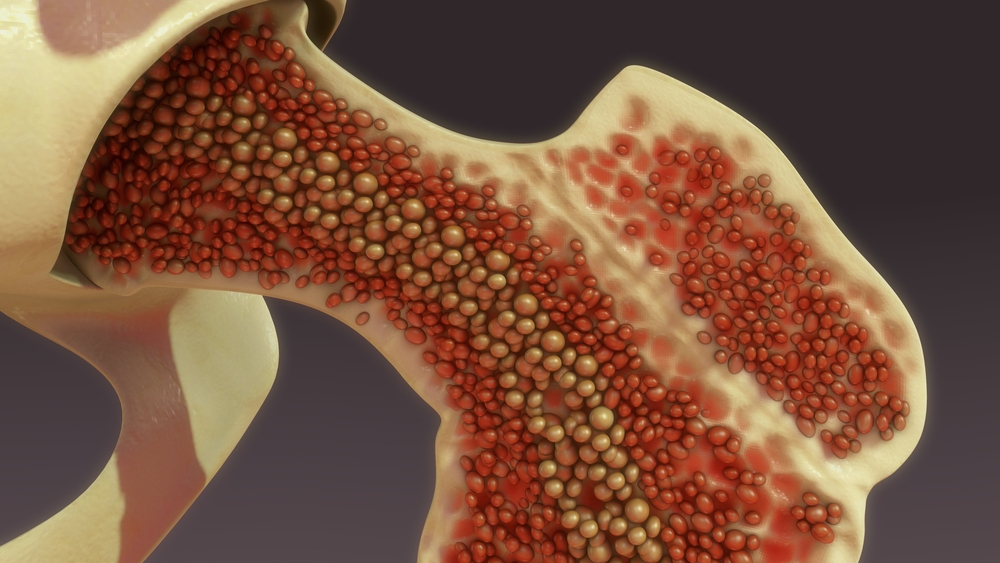
Scientists from Oxford University and the University of Birmingham in the U.K. have made the first bone marrow ‘organoids’ that capture the key features of human bone marrow.
The technology, which is the subject of a patent application filed by University of Birmingham Enterprise, will allow for the screening of multiple anti-cancer drugs at the same time, as well as testing personalized treatments for individual cancer patients.
A study, published in the journal Cancer Discovery, describes the new method, which results in an organoid that faithfully models the cellular, molecular and architectural features of myelopoietic (blood cell producing) bone marrow.
The research also showed the organoids provide a micro-environment that can accept and support the survival of cells from patients with blood malignancies, including multiple myeloma cells, which are notoriously difficult to maintain outside the human body.
Self-organizing cells
Abdullah Khan, a Sir Henry Wellcome Fellow at the University of Birmingham’s Institute of Cardiovascular Sciences and first author of the study, said: “Remarkably, we found that the cells in their bone marrow organoids resemble real bone marrow cells not just in terms of their activity and function, but also in their architectural relationships – the cell types ‘self-organize’ and arrange themselves within the organoids just like they do in human bone marrow in the body.”
This life-like structure enabled the team to study how the cells in the bone marrow interact to support normal blood cell production, and how this is disturbed in bone marrow fibrosis (myelofibrosis), where scar tissue builds up in the bone marrow, causing bone marrow failure. Bone marrow fibrosis can develop in patients with certain types of blood cancers and remains incurable.
Senior study author Bethan Psaila, a hematology medical doctor as well as a research group leader at the Radcliffe Department of Medicine, University of Oxford, said: “To properly understand how and why blood cancers develop, we need to use experimental systems that closely resemble how real human bone marrow works, which we haven’t really had before.
“It’s really exciting to now have this terrific system, as finally, we are able to study cancer directly using cells from our patients, rather than relying on animal models or other simpler systems that do not properly show us how the cancer is developing in the bone marrow in actual patients.”
Cancer treatments
Khan added: “This is a huge step forward, enabling insights into the growth patterns of cancer cells and potentially a more personalized approach to treatment. We now have a platform that we can use to test drugs on a ‘personalized medicine’ basis.
“Having developed and validated the model is the first crucial step, and in our ongoing collaborative work we will be working with others to better understand how the bone marrow works in healthy people, and what goes wrong when they have blood diseases.”
Psaila concluded: “We hope that this new technique will help accelerate the discovery and testing of new blood cancer treatments, getting improved drugs for our patients to clinical trials faster.”
Partnering 2030: The Biotech Perspective 2023