Researchers from King’s College London have succeeded in developing a blood test that can help choose the best treatment for depression patients – a big improvement over the current trial-and-error approach.
 Depression doesn’t seem to be a particularly popular indication for biotechs, unlike other nervous systems diseases that reached significant milestones in the last year. Moreover, one of the few programmes for the disease had a recent Phase II failure.
Depression doesn’t seem to be a particularly popular indication for biotechs, unlike other nervous systems diseases that reached significant milestones in the last year. Moreover, one of the few programmes for the disease had a recent Phase II failure.
Now, researchers at King’s College London have made a breakthrough in the field – not in a novel therapy but for a more effective diagnosis.
Published in the The International Journal of Neuropsychopharmacology, their work shows how a blood test can accurately and reliably predict whether depressed patients will respond to common antidepressants.
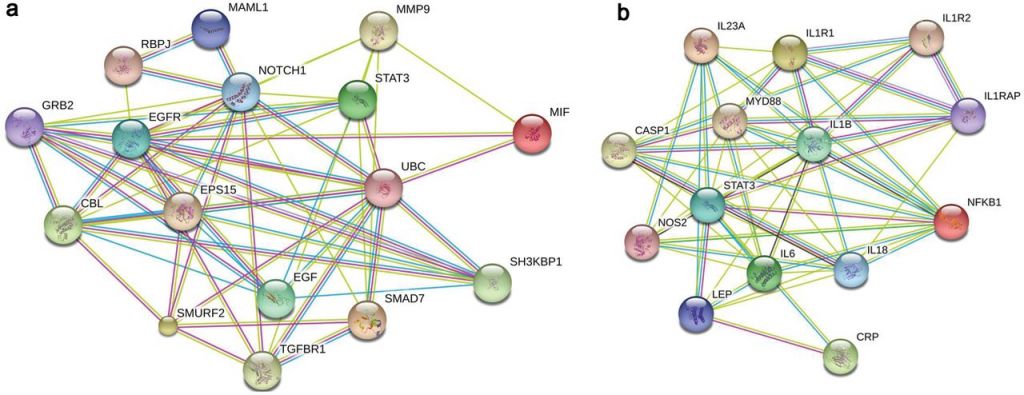
The blood test is based on previous scientific findings of how high levels of inflammation are associated with poor response to antidepressants. The test analyses two biomarkers of inflammation that can be present in the blood – Macrophage Migration Inhibitory Factor (MIF) and interleukin 1-beta (IL-1β).
These biomarkers are involved in several brain mechanisms relevant to depression, including the creation of new brain cells and connections between them.
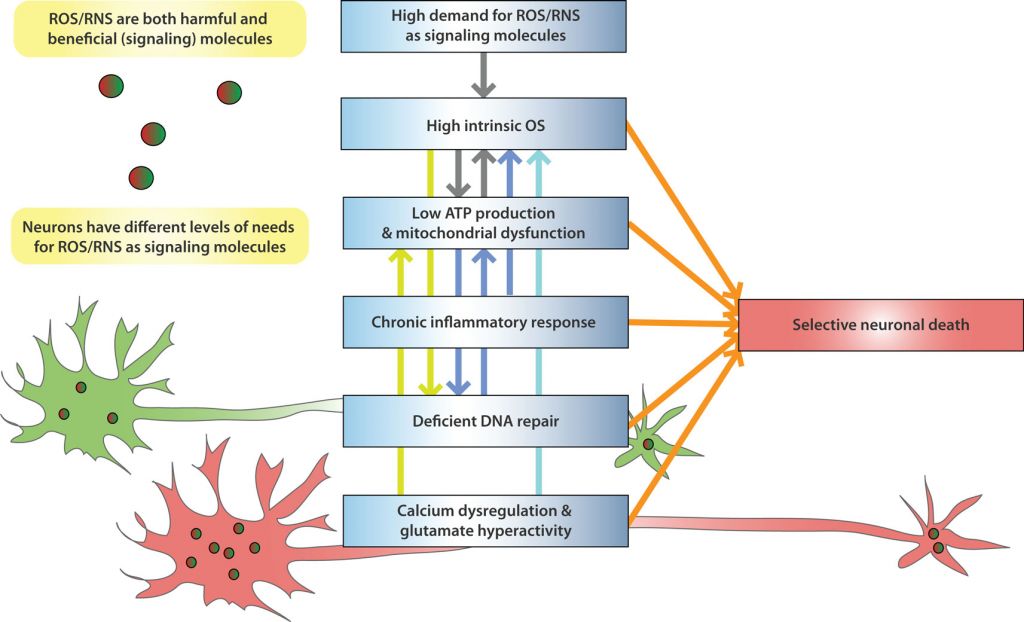
They also relate to oxidative stress, when the body overproduces and then struggles to remove free radicals, molecules that break down brain connections and disrupt the brain’s chemical signaling. This can lead to the development of depressive symptoms.
Patients with high quantities of these biomarkers could now be immediately prescribed stronger medication, as the first-line antidepressants are unlikely to have any effect.
This is a significant improvement over the current trial-and-error approach to depression treatment, where one antidepressant is tried after another with long periods with no symptom improvement in between.
Biomarkers are becoming essential as treatments shift to a more personalized approach. We have already discussed how they are essential to the future of immuno-oncology and seen how they can impact the market cap of biotechs.
For example, there are several diagnostics for particular types of cancer, such as hard-to-treat breast cancer, colorectal cancer and brain cancer and even a universal test for all cancers.
This first diagnostic blood test for depression will not only improve the treatment for this disease (one of the biggest healthcare burdens in Europe), it also proves the versatility of personalized medicine – a key disruption trend in healthcare.
Feature Image Credit: Pixabay
Figure 1 Credit: Cattaneo et al. (2016) Absolute Measurements of Macrophage Migration Inhibitory Factor and Interleukin-1-β mRNA Levels Accurately Predict Treatment Response in Depressed Patients. International Journal of Neuropsychopharmacology (doi: 10.1093/ijnp/pyw045)
Figure 2 Credit: Wang and Michaelis (2010) Selective neuronal vulnerability to oxidative stress in the brain. Frontiers in Aging Neuroscience (doi: 10.3389/fnagi.2010.00012)





