Researchers from Leiden University Medical Center (LUMC) and ISA Pharmaceuticals (Netherlands) have authored an extensive review of what is working in immuno-oncology – and what hasn’t.
 The review was accepted in the well-known journal Nature Reviews Cancer and it covers the findings of 250 peer-reviewed papers about immunotherapies.
The review was accepted in the well-known journal Nature Reviews Cancer and it covers the findings of 250 peer-reviewed papers about immunotherapies.
Immuno-oncology is radically changing the way cancer is being treated, and there are many pharma and biotechs actively pursuing therapies that can turn the patient’s immune system against cancer. However, the actual application of immuno-oncology has a mixed track record. This new review should help understand what strategies are having success.
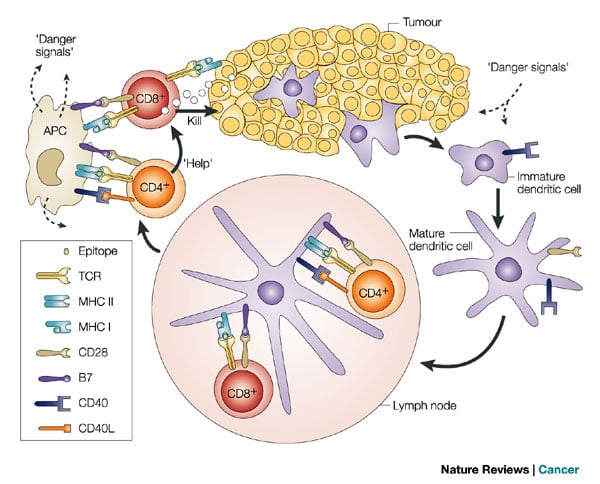
Raising tumor-specific T-cells to target tumors is successful in most cases. However, doing so does not necessarily mean that T-cells can perform their function within the tumor, and effectively destroy it.
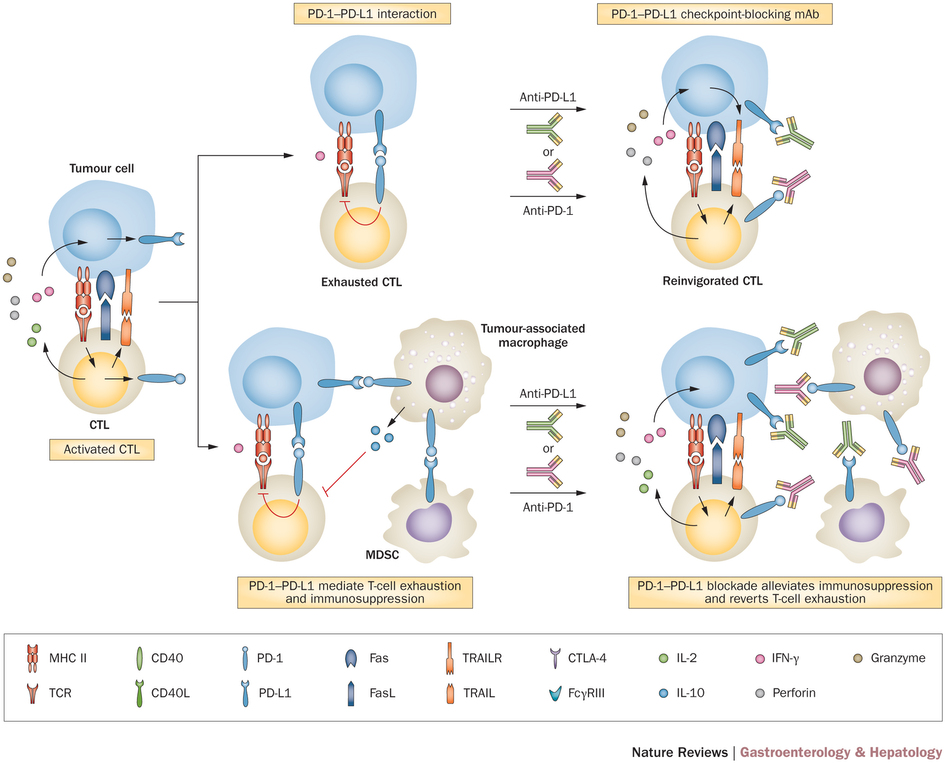
This is because of the overwhelming resilience of cancer cells. They protect themselves by suppressing the immune system. Cancer immunotherapies have only successfully eradicated tumor cells in a setting where immunosuppression was less evident — or counteracted by co-treatments.
So what makes a winning immunotherapy?
The review contains key insights into what successful immunotherapies have in common. It comes down to three main factors.
The first is the selection of tumor-associated antigens, which depends on the type of cancer. In case of virus-induced cancers (like HPV), the antigen should be also from the virus, whereas for cancers of other origins, neo-antigens (arising from mutations in the tumor cells) should be used.
The second part of immunotherapy design is creating a suitable platform that can induce the right immune cells — a robust and balanced ratio of effector cells, as well as the generation of memory T-cells.
As for the last part, successful immunotherapies target the immunosuppressive strategies of tumor cells, including the formation of a ‘tumor microenvironment‘. This can be done via specific co-treatments, such as chemotherapy or checkpoint blocking, with the immunotherapy.
Chemotherapy ‘irritates’ the immune system to the point that it will act even in the immunosuppressive microenvironment inside the tumor — a sort of physiological tug-o-war. If chemo wins out, the immunotherapy will have gained the conditions to act.
As for checkpoint blocking, it is a strategy that blocks the natural ‘safety checks’ of the immune system. These are (of course) very useful when a person is dealing with other types of disease, as it stops the immune response from going into overdrive and damaging collateral healthy tissue.
But cancer cells can hijack this system to escape the immune system — and immunotherapies. So a way to increase the effectiveness of immunotherapies is to block the checkpoints.
The review shows that immunotherapeutic vaccines alone can be used to treat cancer in some conditions. These are cases of premalignant disease, carcinoma in situ or minimal residual disease. However, in progressive cancers, immunotherapies take the role of helpers, rather than the cure. They can increase the effectiveness of other treatments, like chemotherapy.
These insights from previous works could guide the development of more effective immuno-oncology therapies…
Images via Lymphocytes © Animaxx3d (BigStock ID68894674); Tindle (2002) Immune evasion in human papillomavirus-associated cervical cancer. Nature Reviews Cancer (doi: 10.1038/nrc700); Prieto et. all (2015) Immunological landscape and immunotherapy of hepatocellular carcinoma. Nature Reviews Gastroenterology and Hepatology (doi: 10.1038/nrgastro.2015.173)