Stay up-to-date with the latest news related to CAR-T therapy. Subscribe to our newsletter.
What is CAR-T therapy?
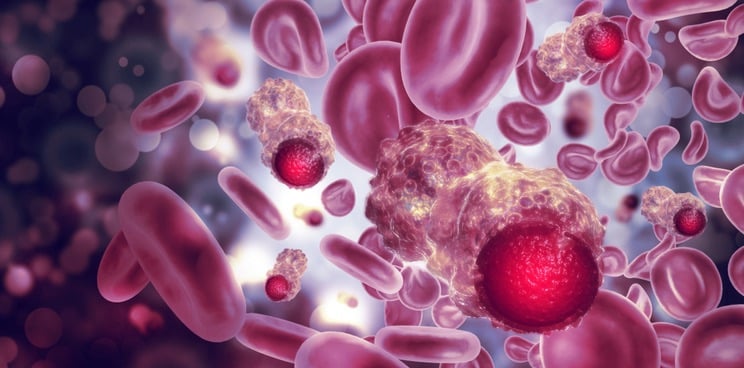
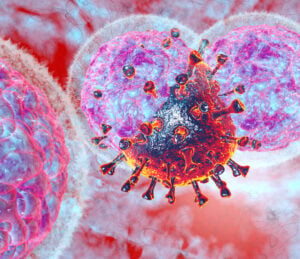
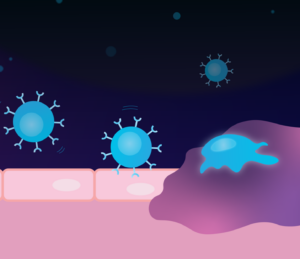
CAR-T (Chimeric Antigen Receptor T-cell) therapy is a form of immunotherapy that involves extracting a patient’s T-cells, genetically modifying them to target cancer cells, and then infusing them back into the patient’s body to attack cancer cells.
What are the applications of CAR-T therapy?
CAR-T therapy applications include the treatment of blood cancers, such as leukemia and lymphoma, that have not responded to other treatments. Researchers are also exploring the use of CAR-T therapy for the treatment of solid tumors. CAR-T therapy represents a promising new approach to cancer treatment that has shown impressive results in clinical trials.
Got a news story for us related to CAR-T therapy? Send it to us here.