Stay up-to-date with the latest biotech news related to cancer. Subscribe to our newsletter.
What is cancer?
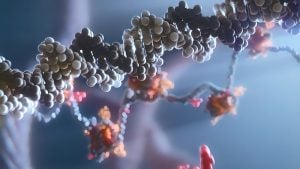
Cancer is a disease characterized by the uncontrolled growth and spread of abnormal cells in the body. These cells can form tumors and invade nearby tissues and organs, interfering with their normal functions. Cancer can occur in almost any part of the body.
How is biotechnology revolutionizing the treatment of cancer?
Biotechnology is transforming cancer treatment with targeted therapies, immunotherapies, and personalized medicine. Companies are using cutting-edge technologies like gene editing and AI to improve therapies and identify biomarkers for personalized treatment. The result is more effective, less invasive, and individualized cancer treatment that is revolutionizing oncology.
Got a news story for us related to cancer research? Send it to us here.