Swedish researchers have found that insulin-producing cells alone are not enough to fine-tune blood sugar levels. This could change the way diabetes treatments are designed.
While it is known that certain clusters of cells in the pancreas called pancreatic islets influence the set point for blood sugar, the exact mechanisms are still unknown. The control of blood sugar levels is a complex process that involves multiple organs, including the pancreas, liver and brain. An imbalance in blood sugar levels can lead to diabetes.
Researchers at the Karolinska Institutet in Stockholm, Sweden, have found that the hormone glucagon secreted from alpha cells is needed in addition to insulin-producing cells to fine-tune the ideal blood sugar level, called the set point, in humans but not in mice.
To investigate the mechanisms behind blood sugar regulation, the researchers took pancreatic islets from different species, including humans, and transplanted them into diabetic and non-diabetic mice. Afterwards, they measured the blood sugar levels and sugar tolerance of the mice.
When human pancreatic islets were transplanted into mice, the mice’s blood sugar levels rose to the human set point. Two key hormones regulate blood sugar: insulin, which decreases blood sugar, and glucagon, which increases blood sugar. Importantly, the researchers found that glucagon input from an alpha cell to an insulin-secreting beta cell within a pancreatic islet is necessary to adjust the human set point.
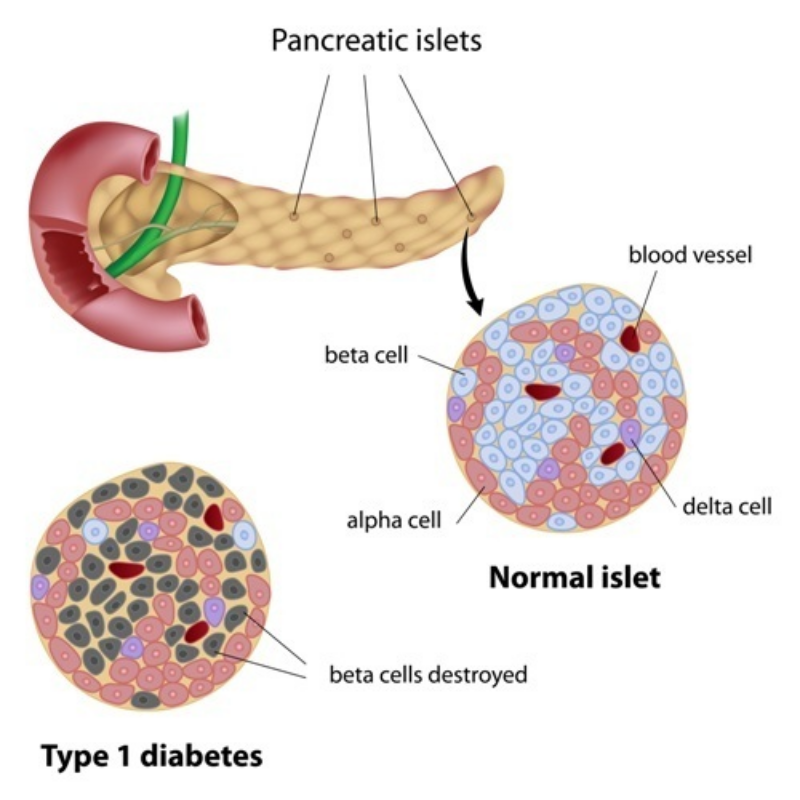
For biotechs, these findings mean that preclinical results in mice do not necessarily translate to humans. Treatments in development need to consider the effect of glucagon release from alpha cells in addition to insulin produced by beta cells for greater efficacy.
Novo Nordisk and Zealand Pharma are already doing this. The Danish companies have both partnered with US-based Beta Bionics to develop the iLet artificial pancreas for type 1 diabetes, which adjusts the amounts of insulin and glucagon delivered every five minutes.
Additionally, the Swedish research also implies that stem cell treatments for diabetes may need to create pancreatic islets with multiple cell types in order to fully restore blood glucose regulation in patients. London-based biotech Catapult is doing just that with its laboratory-grown pancreatic islets, known as Islexa, for patients with type 1 diabetes.
The biotech industry is rife with other novel cell therapies being developed to treat diabetes. For example, French biotech Poxel is developing a treatment that targets the mitochondria of protect-beta cells, which secrete insulin and make up the majority of cells in pancreatic islets.
Research like the Swedish team’s is imperative to developing a fuller understanding of diabetes disease mechanisms and therefore designing treatments that have a greater chance of working in patients.
Images by yodiyim, Alila Medical Media/Shutterstock