Newsletter Signup - Under Article / In Page
"*" indicates required fields
This article was originally published in April 2020, and has been updated with the latest in phage therapy.
Antibiotic-resistant superbugs cause a large number of deaths around the world each year, but effective new antibiotics are thin on the ground. Could bacteria-eating phage viruses be the answer to this problem?
The COVID-19 pandemic has received blanket news coverage over the past couple of years, however, it still pales in comparison to the threat posed by antibiotic-resistant superbugs.
As of August 2022, more than 6 million people worldwide have died as a result of COVID-19, but it’s estimated that antibiotic resistance contributes to almost 5 million deaths globally every year. With bacteria continuing to evolve and render currently available antibiotics useless, this annual death toll is predicted to rise to 10 million by 2050 unless solutions are found.
This problem could also have an impact on other parts of healthcare such as cancer treatment. Already studies have identified a rise in superbud infections in cancer patients. Because of the threat of these opportunistic infections, some oncology treatments may become obsolete within the next decade.
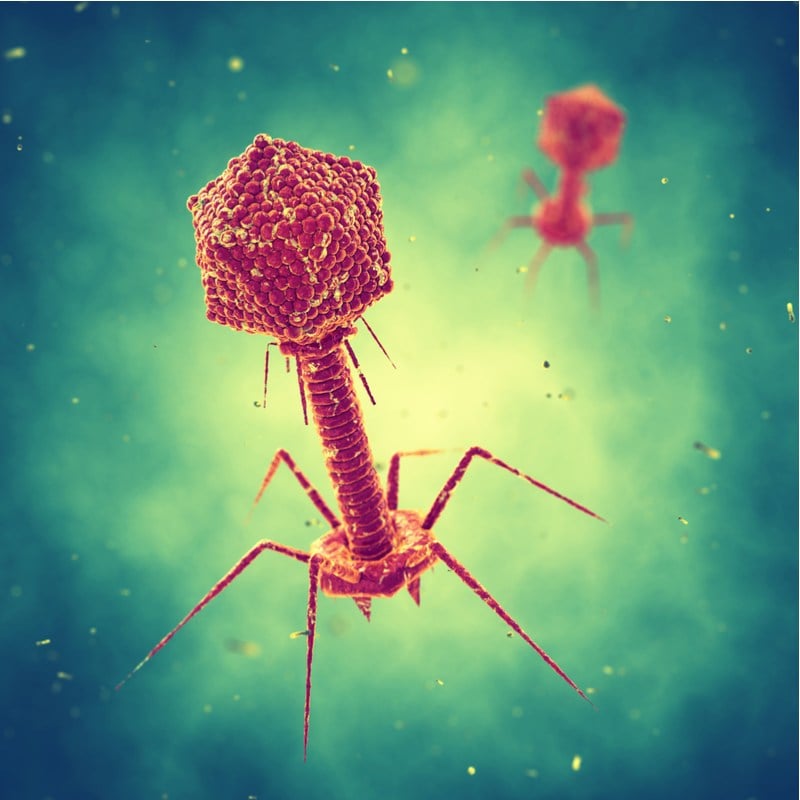
But, there is one solution that could stop superbugs in their tracks; one that has already been known for more than a century. Phages – viruses that parasitize bacteria – were first discovered in 1917, but the complexity of using them therapeutically meant they soon fell out of favor in Europe and the U.S. following the discovery of penicillin and other antibiotics.
The urgency of the antibiotic resistance crisis has led to a resurgence of interest in these largely long-forgotten treatments. Many biotechs believe that technological advances over the past decade have made it feasible to develop commercial phage therapies to treat a range of conditions.
“Developing a phage drug would not have been possible a decade ago,” said Lorenzo Corsini, managing director of BioNTech R&D (Austria). This firm used to be known as PhagoMed, an Austrian phage therapy company, but was acquired by BioNTech in late 2021.
“You need cheap sequencing of many phages and bacterial strains, and that has become available only recently. Now there are several promising candidates in the pipelines of various biotechs which make use of these under-utilized natural bacteria-killers.”
Making phages commercially viable
One of the hurdles to rolling out phage therapies on a large scale has always been that phages are picky eaters. While there are trillions of them out there, each phage is only attracted to specific strains of bacteria, so identifying a cocktail of phages to target a particular patient’s infection is a laborious and expensive process. This means that thus far, phages have mainly been used in last-resort cases where no other treatment has worked.
“Designing a broadly applicable phage product is tricky as every patient has slightly different strains of bacteria,” explained Jonathan Solomon, CEO of Israeli biotech BiomX. The company is developing customized phage therapies to target harmful bacteria causing infections in cystic fibrosis patients, with other programs to treat the skin condition atopic dermatitis acne as well as inflammatory bowel disease and colorectal cancer.
“The key is to identify and optimize a combination of phages that can potentially target as many of these different strains as possible. This is quite a daunting task that requires advanced technologies such as robotics, bioinformatics, and at times, synthetic biology.”
A decade ago, many of these technologies were not available. But such advancements now allow phages to be created in the lab through genetic engineering techniques. Scientists can effectively design phages to have a range of desirable properties such as a wide bacterial target range, and being better at dissolving the cell walls of their target bacteria. The best-engineered phages are combined into potent cocktails.
There are no approved phage therapies in the U.S. or EU, though some such therapies are used on a limited basis for compassionate use in desperate cases. The most advanced candidates globally are in early clinical testing, led by firms including Armata Pharmaceuticals, BiomX, Adaptive Phage Therapeutics and Pherecydes Pharma.
Quelling the skepticism
It isn’t just new technologies that are required for phage therapy to reach prime time; there is still a considerable amount of skepticism to be overcome. Within the medical community, these treatments are still regarded as last-ditch throws of the dice, not to be tried until the last antibiotic has failed.
Corsini feels that for these perceptions to change, it is necessary for the biotech industry to develop a phage-based product that has such distinct advantages over currently available treatments that it would become an automatic choice. One particular area of need is infections associated with medical implants. These are mostly caused by a genus of bacteria called Staphylococcus, and are a dreaded complication for surgeons as the microbes form biofilms that cannot be penetrated by antibiotics.
“The current standard of care is removing the biofilm surgically, often including the whole implant, because there is no known antibiotic that does the job,” says Corsini.
“However, phages have evolved to attach to biofilms. They even have special enzymes that degrade the extracellular matrix, a slimy layer that protects the cells in the biofilm. This makes it feasible to create a fixed, off-the-shelf cocktail that could tackle these infections.”
While Corsini is bullish about the prospect, the reproducibility of such an off-the-shelf product in clinical settings remains yet to be proven.
This is why Pherecydes – a French biotech developing phage therapies for a range of different conditions – is taking a different approach. Rather than attempting to produce a product that can be given to any patient, its therapies are individualized to the patient. The company does this by first conducting a detailed preliminary analysis of the patient’s bacterial infection, and then tailoring the phage cocktail to the infection profile.
Pherecydes’ approach could be more financially viable than current methods of administering phase therapy to patients because the company’s phages are produced in large batches, and so can be given to any patient with a similar strain.
“We have developed the concept of precision phage therapy whereby patients are treated with phages that are active on their bacterial strain,” explained Guy-Charles Fanneau De La Horie, former CEO of Pherecydes.

“This can be achieved in less than 48 hours, and fits with the current modus operandi of the hospitals,” De La Horie continued. “Our phages have been administered intravenously to patients with no reported side effects.”
Futuristic plans
The continued emergence of new technologies like CRISPR may well eventually lead to even more futuristic applications of phage therapy. One idea being researched by academics in the U.S. is to use CRISPR-Cas9 as a way of genetically engineering phages so they have a much wider range of preferred bacteria to munch on. The concept seems promising, although as De La Horie points out, getting such a product licensed by regulators would be a challenge.
“The product to be administered to patients would be a genetically-modified organism and we believe it would be a real challenge in Europe to get that authorized,” he explained.
In addition, an increasing number of scientists are now researching the microbiome and the role of certain bacterial species within the gut in contributing towards various disorders. BiomX believes there could be a role for phage therapy in tackling some of the underlying causes of chronic disease, particularly as more of these gut microbiota species are identified.
BiomX is collaborating with a group of academics at Keio University in Tokyo that has identified specific strains of a bacteria called Klebsiella pneumonia as playing a pivotal role in inflammatory bowel disease. By inducing an inflammatory response, the team has been able to develop a phage cocktail targeting these bacteria. This cocktail showed promising safety results in a phase Ia trial, as well as showing the phage was delivered successfully to the lower gastrointestinal tract.
However, one of the key issues facing all biotechs developing phage therapies is one of financing. De La Horie points out that the economics of developing therapeutics for bacterial infections is challenging. Many companies that brought new antibiotics to the market in the past decade have gone bankrupt, such as the US companies Melinta Therapeutics and Achaogen.
De La Horie believes that ultimately governmental intervention is required to ensure that producing a pipeline of antimicrobial therapies remains financially viable.
“With phages, there is clearly a need for such treatments,” he emphasized. “The sooner they will be on the market, the better for patients who can benefit from them. We do receive frequent requests from French hospitals for such treatments, which demonstrates the need.”
There are some signs that governments are listening to the calls for change in how we tackle antibiotic resistance. Earlier this year, the U.K. began a program where companies that commercialize antibiotics are paid in a subscription model, rather than only when the antibiotics are used. The first beneficiaries of the model were two new antibiotics made by Pfizer and Shionogi.
If policies like that of the UK succeed, this could show promise for the future of companies developing other solutions to the superbug crisis, including phage therapies.






