Newsletter Signup - Under Article / In Page
"*" indicates required fields
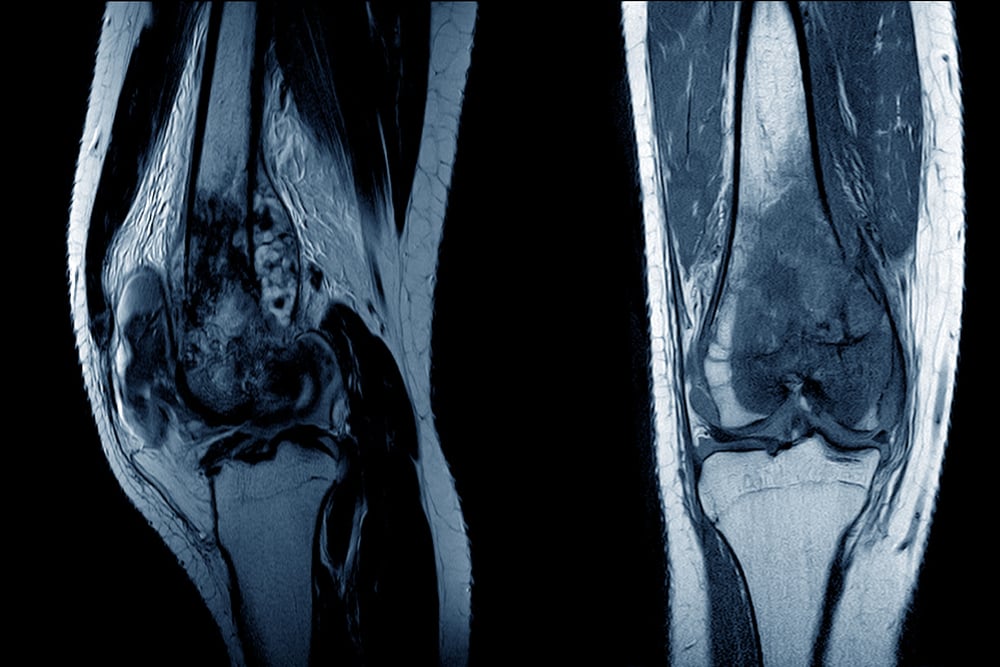
New research has identified a potential therapeutic target and developed a unique delivery system to treat osteosarcoma, a bone cancer that primarily affects children and adolescents.
The standard-of-care treatment plan for osteosarcoma today is no different to when first introduced almost 50 years ago. However, nearly one third of patients’ relapse and need new interventions. This prompted Fiona Freeman, assistant professor, UCD School of Mechanical and Materials Engineering and Fellow, UCD Conway Institute, in Ireland, to focus on the possible use of microRNA therapy in osteosarcoma, and specifically on a molecule called miR-29b.
MicroRNAs are a family of molecules that help control certain activities in cells like growth and development. They are showing promising results in the treatment of cancer and viral infection. This study introduces for the first time, the therapeutic potential of miR-29b in blocking osteosarcoma tumor growth and the potential of nanoparticles as a therapeutic delivery vehicle to treat the cancer.
Suppressing tumor growth
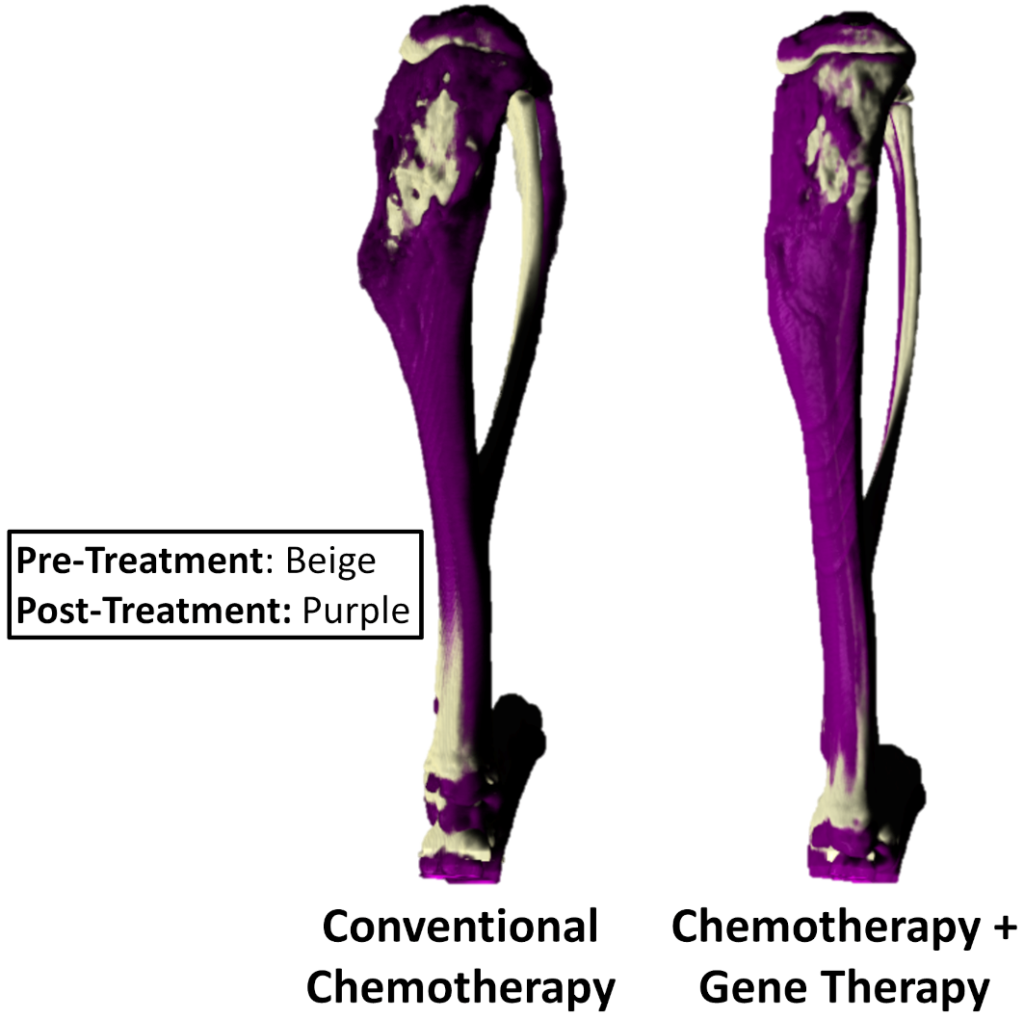
“The main findings from our study demonstrated that when locally administered via an injectable delivery system, our miR-29b loaded nanoparticles improved the therapeutic potential of chemotherapy and suppressed tumor growth while simultaneously aiding in the repair of the surrounding damaged bone even while the patient is undergoing chemotherapy treatment,” said Freeman, who led the study.
The current gold standard treatment option requires extensive surgical intervention and chemotherapy that leads to a poor prognosis and decreased quality of life. Due to the aggressive nature of the disease, the surgical intervention usually involves total reconstruction of the limbs or in most cases amputation.
To add to this, both chemotherapeutics and osteosarcoma tumors have been shown to disrupt bone ability to repair following surgical intervention.
“Any bone regeneration strategy that would aid in the regeneration of the damaged bone would be of great benefit to these young patients so that they don’t lose their limbs. Yet, there is a fine balance between trying to promote bone regeneration and promoting tumor growth, which has significantly slowed fundamental research and clinical translation of tissue engineering strategies for cancer patients.”
The team developed a formulation of miR-29b:nanoparticles that were delivered via a hyaluronic-based hydrogel to enable local and sustained release of the therapy.
Approaches to eliminate osteosarcoma
“This work is seeking to answer an important basic science question, as to the balance between inducing tissue regeneration and preventing tumor recurrence, and how gene therapy approaches can help eliminate osteosarcoma in combination with standard chemotherapy,” said Natalie Artzi, an associate professor in Brigham Women’s Hospital and Massachusetts Institute of Technology, who was senior author of the report.
The hyaluronic-based injectable delivery system turned to gel at the target area of the body in a matter of minutes and allowed for local and sustained delivery of the miR-29b to the primary tumor site. Clinicians would be able to inject directly into the defect site during the procedure to remove the tumor, as no UV or temperature is needed for gelation. So, this localized therapy has the potential to be integrated into the current clinical treatment regime as an add-on to conventional chemotherapy. This could further improve clinical outcomes for these young patients.
The research team also validated the therapeutic potential using two predictive models of the disease; a 3D co-culture spheroid model; and an orthotopic metastatic murine model.
“Fiona’s findings have the potential to revolutionize cancer treatment and improve outcomes by providing vital information that can inform the design of future combination therapies for these young patients,” said Daniel Kelly, a professor in tissue engineering at Trinity College Dublin and Amber principal investigator, who was co-author of the report.
Importance of lung metastasis
On the potential next steps for this research, Freeman said: “This innovative microRNA therapy could potentially be administered to osteosarcoma patients immediately after cancer diagnosis, before surgical intervention, to reduce spread of the tumor to other sites in the body (metastasis), which is critical in patients’ survival.
“Lung metastasis is the most critical clinical factor. 70% of patients who develop lung metastasis succumb to the disease within three years. This therapy could significantly impact the overall survival rate of these young patients. The therapy could be applied locally, following surgery to eliminate remaining malignant cells that could cause tumor recurrence while repairing the damaged bone during chemotherapy, providing an essential alternative to prevent limb amputation.”
Oncology R&D trends and breakthrough innovations