Newsletter Signup - Under Article / In Page
"*" indicates required fields
In an early study at Queen Mary University in London, a modified flu virus has been able to block the growth of pancreatic cancer.
For the first time, researchers at Queen Mary University, London, have shown that pancreatic cancer can be targeted using a modified flu virus. During a study, published in Molecular Cancer Therapeutics, a modified flu virus was developed that targets a unique feature of pancreatic cancer cells. The approach showed potential as a future treatment of the disease as it blocked tumor growth in mice.
Pancreatic cancer is particularly difficult to treat due to late diagnosis and the rapid development of resistance to current therapies. This contributes to a particularly low 10-year survival rate of less than 1% and it being the fourth biggest cause of death in Europe. At the moment, the best – and most expensive – way to survive is to undergo a pancreatic transplant as Steve Jobs did.
The group found a molecule, alpha v beta 6 (αvβ6), that is only found on the surface of pancreatic tumors. This prompted them to develop an oncolytic virus that expresses an extra protein that recognizes and binds αvβ6. This allows the virus to enter cancer cells, replicate itself many times, and burst out, destroying its host in the process. Newly produced viruses can then bind neighboring cells and repeat the process to remove the whole tumor.
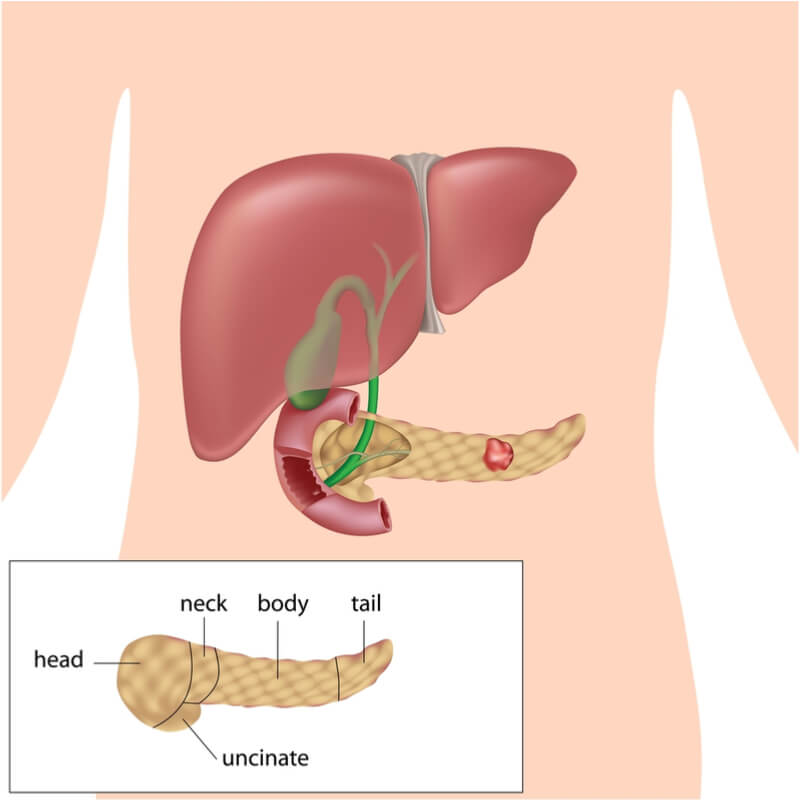
The virus was tested on human pancreatic cancer cells in mice and found that they effectively inhibited cancer growth. Oncolytic viruses are not a new approach to cancer treatment but the researchers believe that their new virus is more specific and effective – plus, it can be used in combination with current chemotherapy drugs.
Biotechs may well have been forced to think outside the box due to the difficulty in treating pancreatic cancer, leading to the development of some interesting approaches. Examples include Erytech’s armed red blood cells, which are headed for Phase III, Targovax’s peptide vaccine that kept all Phase I/II study patients alive after 1 year, and 4SC’s epigenetics drug, resminostat.
The development of better diagnostic techniques should also help to boost the disease’s dismal survival rate. Liquid biopsies are moving away from invasive solid tissue sampling, and British biotech ANGLE’s Parsortix system is already showing promise for other indications like prostate cancer.
Images – Dina van Wyk / shutterstock.com; Alila Medical Media / shutterstock.com
Oncology R&D trends and breakthrough innovations







