Newsletter Signup - Under Article / In Page
"*" indicates required fields
SMART102, a human T-lymphoid progenitor cell injection derived from cord blood using Smart Immune’s ProTcell platform, has entered clinical testing.
The trial is being sponsored and led by Great Paris University Hospitals (AP-HP).
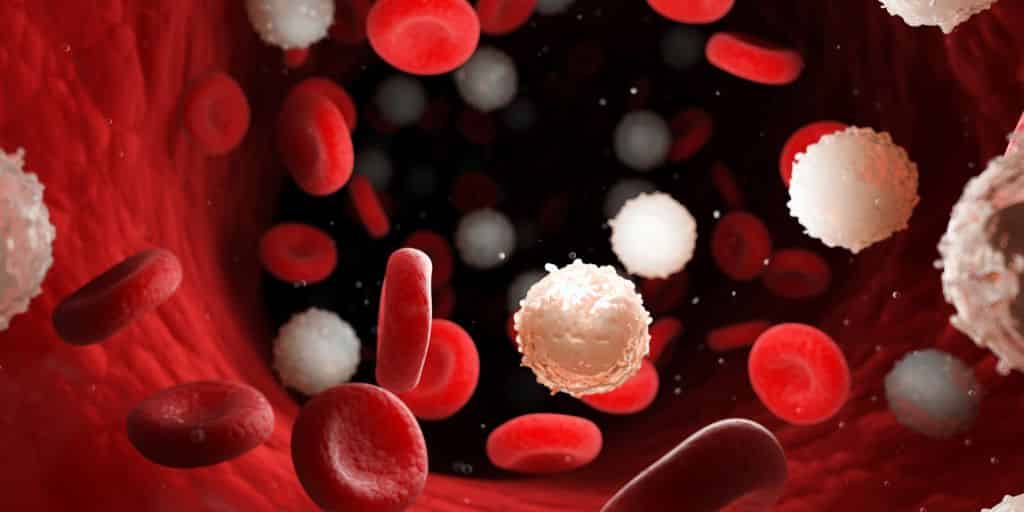
Smart Immune SAS is a clinical-stage biotechnology company developing ProTcell, a thymus-empowered T-cell therapy platform to fully and rapidly re-arm the immune system.
The multicenter phase I/II trial (NCT04707300) is a proof-of-concept, dose escalation, 10-patient study that will evaluate the safety and efficacy of SMART102 to accelerate immune reconstitution after allogeneic hematopoietic stem cell transplantation (HSCT) in adult patients with hematological malignancies.
SMART102 is an injection into the patient of allogeneic T-cell progenitors produced by Smart Immune’s ProTcell platform designed to travel to the patient’s thymus and become differentiated into fully functional T-cells.
The trial has been designed to assess the potential of the ProTcell technology to improve clinical outcomes of HSCT. Overall survival in this patient group is currently low at five years post-HSCT, with around 50% mortality.
No safety-related issues or dose limiting toxicity have been reported in the first patient enrolled in the trial to date. Preliminary data from the trial are expected in around 18 months.
Reduction in time
Karine Rossignol, co-founder and chief executive officer of Smart Immune, said: “This trial follows the pioneering work of our co-founders Professor Marina Cavazzana and Dr Isabelle André and their teams at Necker Children Hospital, AP-HP and the Imagine Institute.
“Smart Immune can develop large numbers of T-cell progenitors from hematopoietic stem cells in one week ex vivo, which the thymus ‘educates’ to become the full repertoire of immune cells in around three months, compared with 15-18 months through bone marrow transplantation alone. This significantly reduces the time to full immune recovery and potentially provides a transformational shift in the benefit/risk ratio of allogeneic T-cell medicine.”
Olivier Hermine, head of hematology at Necker Children Hospital, AP-HP, and principal investigator of the study, said: “Immune reconstitution post allo HSCT remains a huge unmet medical need. Faster, polyclonal T-cell recovery after transplantation will be key to improving clinical outcomes and survival. No therapy to date allows it. We are excited to start addressing it in this first-time-in oncology human trial by using ProTcell from cord blood in combination with unmanipulated cord blood stem cells of a different source.”
Double cord-blood approach
Umbilical cord blood (UCB) grafts are frequently used for patients lacking an HLA-matched family donor and in the absence of an appropriate unrelated donor. As with any HSCT, UCB transplantations are associated with the risk of acute and chronic GVHD (graft versus host disease), post-transplant immunodeficiency with increased risk of infections, as well as relapse. These risks have been linked to a delay in immune reconstitution, and the longer a patient remains without a fully functional immune system, the greater the risks.
This phase I/II trial protocol utilizes two umbilical cord blood units for each patient. One remains unmanipulated and is grafted into the patient on day zero as standard allogeneic cord blood transplantation. On the same day, the patient also receives an injection of SMART102 T-cell progenitor cells, derived from the second unit of cord blood using ProTcell technology.
The aim is to induce faster T-cell reconstitution through ProTcell technology and improve clinical outcomes for this patient population.
The ProTcell platform aims to accelerate the production of tolerized, allogeneic, polyclonal naive T-cells by the patient’s own thymus through infusion of clinical-grade, allogeneic early lymphoid progenitor cells generated in seven days ex-vivo. Preclinical data suggest that the ProTcell platform may reconstitute the immune system in 100 days instead of the 12 to 18 months observed in physiology.
Oncology R&D trends and breakthrough innovations