By Dr. Alexander Zehnder, CEO, CureVac
The success of mRNA vaccines in COVID-19 propelled the role of this new modality to the forefront of medicine. Not only are new prophylactic mRNA vaccines for various respiratory diseases advancing through clinical development, but mRNA medicines are now being developed in many wide-ranging applications, including cancer and rare diseases.
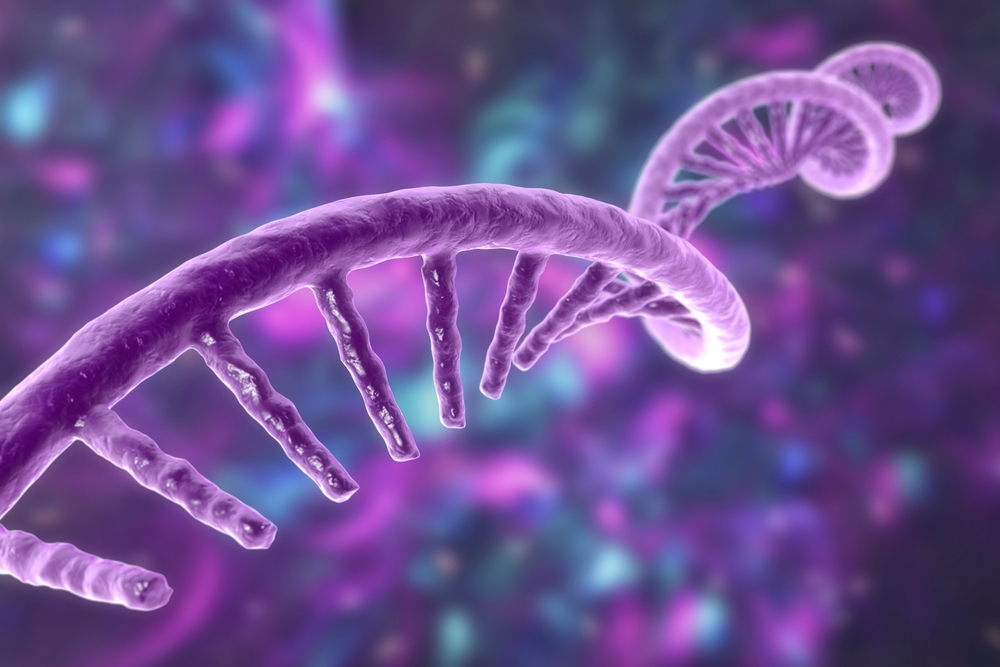
The tremendous therapeutic potential of mRNA lies in its role as an information-carrying molecule that directs protein production in every living cell. Ultimately, mRNA therapeutics enable the body to make its own drugs by mimicking endogenous mRNA. But what is needed to design a potent and successful mRNA vaccine or therapeutic?
Challenges of using mRNA as a medicine
Using mRNA as a medicine has long been of interest given its potential to address limitations of existing treatment modalities. However, mRNA has historically been limited by several theoretical and practical hurdles, namely:
- Stability: Naked mRNA is rapidly degraded by RNase enzymes present throughout the environment, limiting the ability to produce stable mRNA therapeutics. Additionally, endogenous mRNA degradation pathways in the body limit the duration of its therapeutic effect. An effective mRNA treatment needs to be masked from these enzymes both as a drug formulation and upon introduction into the body.
- Uptake by cells: While it is possible to deliver mRNA directly into the target tissue without delivery systems in certain cases, the presence of RNA degrading enzymes in blood and interstitial fluids rapidly regrade any extracellular mRNA. A more effective mRNA-based medicine needs a delivery system that delivers mRNA efficiently into cells.
- Expression level: Protein expression levels from synthetic mRNA obtained by in vitro production have historically been considered far too low for therapeutic purposes. This problem could not be overcome until mRNA structural features were developed to significanly increase mRNA expression.
- Immunogenicity: mRNA has the ability to strongly activate receptors on cells as well as sensors within cells. This process triggers the innate immune response and can lead to shut down of protein translation in cells. An effective mRNA-based medicine needs to modulate the immune system according to the targeted disease indication.
The potency of the administered mRNA drug product is the combination of the potential efficacy of the mRNA that encodes the antigen protein and the delivery system that transports the mRNA to the cells. The success of mRNA therapeutics and vaccines can only be achieved when several components are optimized to work efficiently together. These components include the mRNA backbone, an appropriate antigen and a delivery system encasing the mRNA, such as lipid nanoparticle systems (LNPs).
Optimizing the mRNA backbone – the foundation
The principle behind mRNA medicines is to use synthetic mRNA molecules to direct the production of a protein that will generate a desired immune response. The synthetic mRNA strand also contains a number of structural elements that characterize every natural mRNA: a 5′ cap, a 5′-untranslated region (5’UTR), a coding region, or open reading frame (ORF), and a 3′-untranslated region (3’ UTR) including a poly(A) tail.
Optimization of the mRNA backbone targets the generation of the most efficacious mRNA for any particular target and indication by optimizing translation, stability and immunogenicity. Each of these parameters can be modified by changing individual mRNA elements and their interplay guided by the envisaged application.
For example, UTRs contribute decisively to the potential efficacy of mRNA medicines. Depending on the target and indication, the required pharmacokinetics of protein expression might be different.
Some applications may require the highest possible protein expression but only for a limited time, for other applications, long-lasting protein expression might be key. Peak level and duration of protein expression can be adjusted by the choice or design of enhancer and stabilizing elements in the untranslated regions of an mRNA, or the secondary structure of the mRNA molecule. Another example is the optimization of how the ORF instructs the synthesis of the protein it encodes by the ribosome. The ORF sequence can be optimized to increase stability of mRNA. Importantly, this can be achieved without altering the protein sequence encoded by the ORF.
For example, at CureVac, our team discovered that by increasing the content of G and C nucleotides mRNA stability and protein expression can be significantly enhanced , so we patented a strategy that replaces A or U nucleotides at the third position in the open reading frame with G or C nucleotidese. The optimization strategy enabled us to develop a novel mRNA backbone used in CV2CoV, CureVac’s second generation COVID-19 vaccine, to elicit substantially greater humoral and cellular immune responses and provide significantly improved protective efficacy against SARS-CoV-2 challenge as compared with the first generation vaccine in macaques.
Each of the mRNA elements together in combination with the overall sequence influence the degree of activation of the immune system by any particular mRNA. Therefore, design of and optimization of an mRNA backbone always considers multiple factors as well as the whole construct.
Proteins – the immune response stimulator
The next key component is the protein, or rather the instructions to encode and produce the desired protein. The protein is recognized as foreign, so the body mounts an immune response to eliminate it. For example, the COVID-19 vaccines induce an immune response to the spike protein on the SARS-Cov-2 virus surface.
Finding the right target plays a particularly crucial role in cancer mRNA vaccine development. Although tumor cells are derived from normal cells, they contain unique molecules expressed on the cell surface, often mutated, that are involved in driving the cell to be cancerous. These molecules are recognized as foreign by the immune system, which can then mount an immune response against the tumor. The difficult part is identifying the right protein to differentiate healthy cells from those developing into cancer.
Conventional target discovery focused on mutations in the tumor exome, which is the coding part of the genome but only represents about 1.5% of the total genetic information. At CureVac, we take a different approach. We perform whole-genome-sequencing and combine it with short and long-read RNA sequencing. This way the full genomic information of a tumor can be mapped.
Downstream of the sequencing, bioinformatic integrates all the data to retrieve the exact changes in the DNA of the tumor cells compared to healthy cells. Correlation of these data results in the identification of new and potentially antigenic tumor proteins that can be used for cancer vaccine development.
Modified versus unmodified mRNA
There has been much debate about using modified and unmodified mRNA and subsequent successful application, particularly for COVID-19 vaccines. The data obtained by BioNTech and Moderna for their COVID-19 vaccines was compelling and subsequent research conducted by us and others in the field suggests that modified mRNA enables higher doses and thereby higher levels of neutralizing antibodies – an essential characteristic of prophylactic vaccines. Modified mRNA has also shown clinical promise in cancer vaccine development. However, clinical testing of modified as well as unmodified mRNA cancer vaccines is ongoing to also determine best induction of potent T cell responses. This is a critical aspect for cancer applications.
LNPs – the delivery vehicle
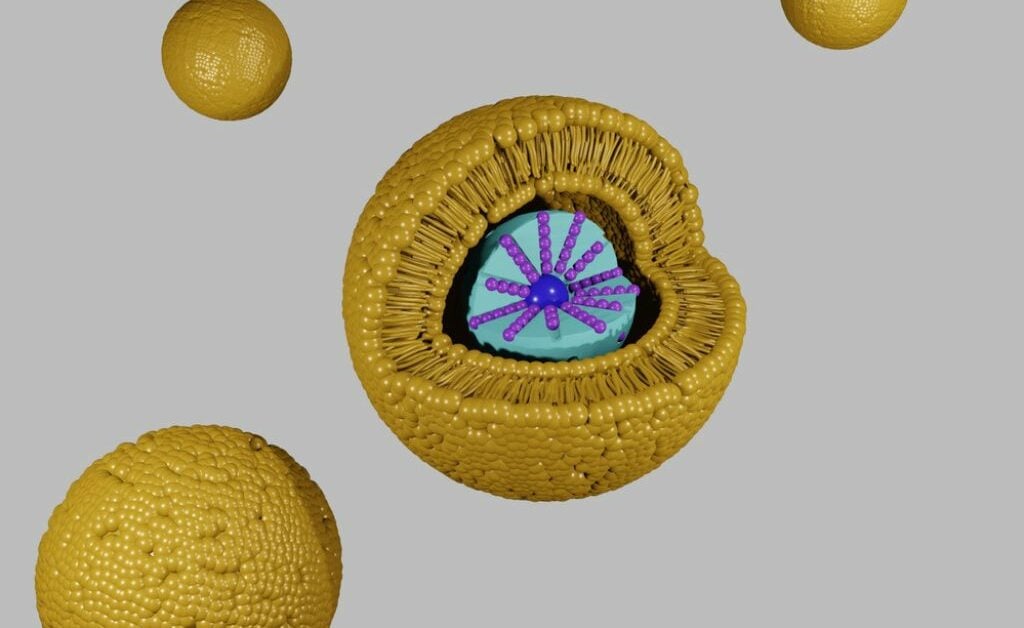
Lastly, LNPs, are the most common and most clinically advanced delivery system used for mRNA products. Encapsulation of the mRNA strand within LNPs enables efficient delivery to the site of action within the cell without being subjected to degradation, rapid excretion and liver clearance. This enables a higher bioavailability and longer half-life.
LNPs consist of different lipids that come together with the mRNA to form a lipid nanoparticle. They mimic low-density lipoproteins, so can be taken up by a cellular transport pathway to deliver the mRNA cargo to cells. At CureVac, we have developed, independently and with commercial partners, multiple LNP technologies. The most important finding in our proprietary LNP research is that the choice of lipids, their composition, and concentration allow us to tailor distinct immune responses. That is a critical aspect to potentially address specific requirements for different applications with bespoke LNP systems. For example, requirements for prophylactic vaccines compared with cancer vaccines are quite different.
LNPs for prophylactic vaccines should primarily support the strong induction of antibodies and minimized reactogenicity as mostly healthy individuals are being
administered. As prophylactic vaccines usually follow seasonal outbreaks, LNPs need to contribute to overall stability of the vaccine for longer-term storage at refrigerator or even room temperature. LNP systems for cancer vaccines on the other hand need to support activation of signaling pathways in the cell for the strong induction of systemic immune responses in seriously ill patients. Activation of certain cytokines and chemokines in those pathways can lead to higher reactogenicity but it is essential for the induction of a T-cell response. For cancer vaccines, stability can be deprioritized in favor of stronger efficacy.
LNP research has shown highly localized distribution in the immune compartments, favorable cellular and humoral immune responses in preclinical tests, as well as early good room temperature stability data as a dried presentation. Biodistribution limited to the immune compartments is particularly important for intramuscular injections to avoid unwanted expression of the antigen in distant organs such as the liver, spleen and lung.
Conclusions: optimizing mRNA medicines
Although much progress in the mRNA field has been made, we need to continue to innovate so that the full promise and potential of mRNA can be realized. Even within the areas of most current knowledge, prophylactic vaccines and cancer, there are almost endless possibilities in designing, optimizing and delivering novel synthetic mRNA medicines.
The future looks bright for this sector, but most of all for the patients that will one day benefit.