Newsletter Signup - Under Article / In Page
"*" indicates required fields
A team of scientists led by Kei-ichi Takata from the Center for Genomic Integrity (CGI) within the Institute for Basic Science (IBS) in South Korea, has discovered a new type of DNA repair mechanism that cancer cells use to recover from next-generation cancer radiation therapy.
Ionizing radiation (IR) therapy is frequently used in the treatment of cancer and is believed to destroy cancer cells by inducing DNA breaks. The newest type of radiation therapy harnesses radiation produced by a particle accelerator, which consists of charged heavy particles such as carbon ions. The particle accelerator accelerates the carbon ions to about 70% of the speed of light, which collides with and destroys the DNA of cancer cells.
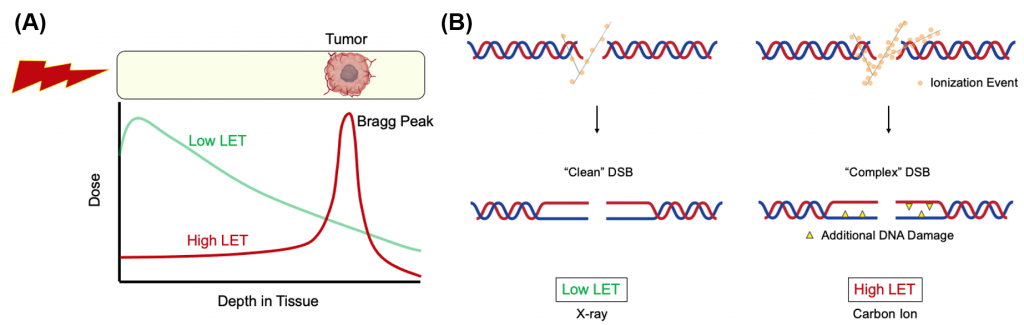
These ions have a high linear energy transfer (LET) and release most of their energy within a short range, called the Bragg peak. The next-generation cancer radiotherapy works by focusing the Bragg peak on the tumor, which has the added benefit of minimizing damage to surrounding normal tissues compared to the commonly used low LET radiation such as gamma or x-rays (Figure 1A).
Only a handful of medical facilities in the world currently possess the capability to deliver this next-generation radiation therapy, although more are hoped to be deployed in the future.
DNA lesions generated by heavy ion bombardment (high LET radiation) are more complex than those induced by traditional radiation therapy (low LET radiation).
The former carries additional DNA damage such as apurinic/apyrimidinic (AP) site and thymine glycol (Tg) in close proximity to the double-strand breaks (DSB) sites, which is far more difficult to repair than ordinary DNA damage. As a result, the advanced therapy is more cytotoxic per unit dose than low LET radiation (Figure 1B).
Cancer cells susceptible to next-generation radiation therapy
This makes next-generation radiation therapy a potent weapon against cancer cells. However, it has not been fully investigated how these high LET-induced lesions are processed in mammalian cells, as DNA damage from heavy ion bombardment is a process that seldom occurs in nature (e.g., higher chance in outer space).
Figuring out the complex DSB repair mechanism is interesting to researchers, as blocking the cancer cells’ repair mechanism can allow the new radiation therapy to become even more effective.
The IBS team visited the QST hospital in Japan to use the synchrotron named HIMAC (Heavy Ion Medical Accelerator in Chiba), which has the ability to produce high LET radiation. A similar synchrotron has been installed at Yonsei University and another is scheduled to be installed at Seoul National University Hospital in Kijang in 2027. Takata’s research team intends to help establish a basic research program using these synchrotrons in South Korea to improve heavy ion therapy in cancer patients.
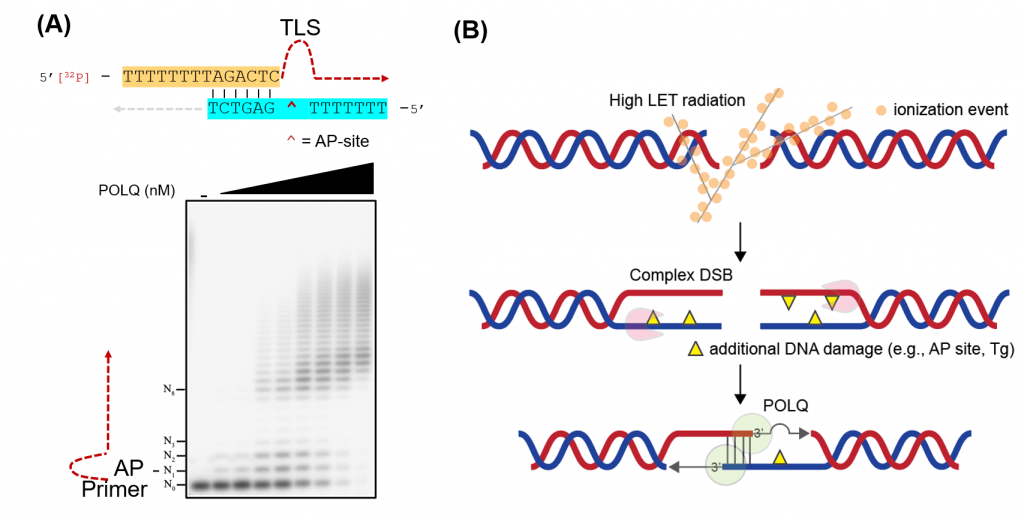
Takata’s group discovered that DNA polymerase θ (POLQ) is an important factor when repairing complex DSBs such as those caused by heavy-ion bombardment. POLQ is a unique DNA polymerase that is able to perform microhomology-mediated end-joining as well as translesion synthesis (TLS) across an abasic (AP) site and thymine glycol (Tg).
This TLS activity was found to be the biologically significant factor that allows for complex DSB repair.
Sung Yubin, one of the joint first authors, said: “We provided evidence that the TLS activity of POLQ plays a critical role in repairing hiLET-DSBs. We found that POLQ efficiently anneals and extends substrates mimicking complex DSBs.” (Figure 2).
Cancer cells and the expression of POLQ
The researchers also discovered that preventing the expression of POLQ in cancer cells greatly increased their vulnerability to the new radiation treatment.
“We demonstrated that genetic disruption of POLQ results in an increase of chromatid breaks and enhanced cellular sensitivity following treatment with high LET radiation,” said Yi Geunil, another joint first author (Figure 3).
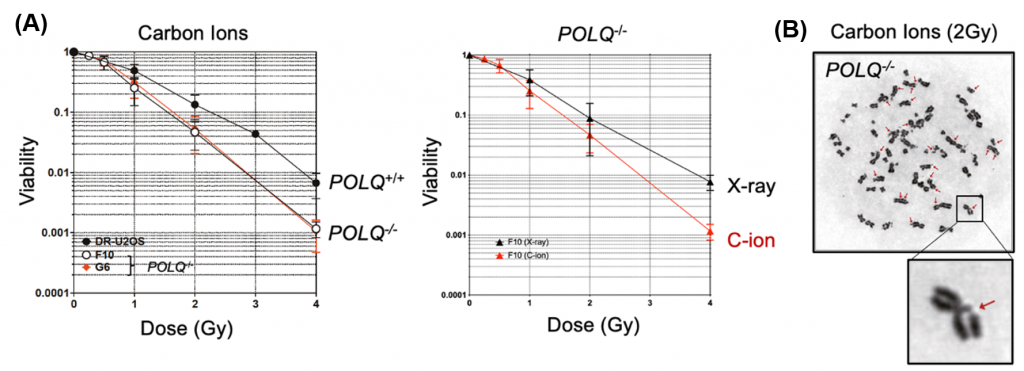
The research team used biochemical techniques and fluorescence resonance energy transfer (FRET) to find out that POLQ protein can effectively repair synthetic DNA molecules that mimic complex DSB. This means that POLQ can be a possible new drug target to increase the cancer cells’ vulnerability against complex radiation damage.
The single-molecule FRET assay system to monitor POLQ-mediated annealing and DNA extension was developed in collaboration with Kim Hajin and Kim Chanwoo at UNIST. Ra Jae Sun at IBS-CGI analyzed chromatid breaks induced by high LET radiation. Fujimori Akira and Hirakawa Hirokazu at QST, and Kato Takamitsu at Colorado State University helped conduct the experiments with HIMAC.
Takata concluded: “We are proud to announce the publication of our paper which was only possible through the great teamwork of everybody involved. Our findings provide new insights into the mechanisms of how hiLET-DSB is repaired in mammalian cells and further suggest that the inhibition of POLQ may augment the efficacy of heavy ion radiation therapy.”
The study was published in Nucleic Acids Research.
The research has implications regarding finding new treatments, and the area of preventing cancer cells from repairing their DNA is already being investigated. Hamburg-based Evotec spinout Breakpoint Therapeutics is working on cancer treatments that block the ability of tumor cells to repair their own DNA.
Oncology R&D trends and breakthrough innovations