Newsletter Signup - Under Article / In Page
"*" indicates required fields
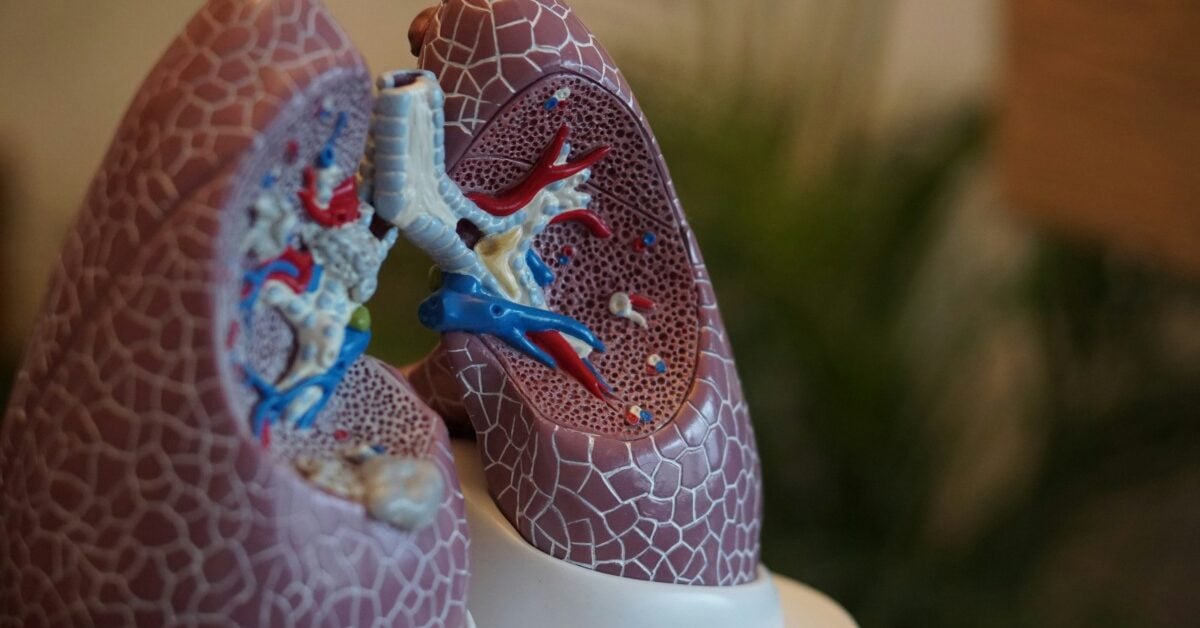
Cystic fibrosis is a condition that causes sticky mucus to build up in the lungs and digestive system. This causes lung infections, problems with digesting food, and severe damage to several organs in the body.
There are nearly 40,000 children and adults living with cystic fibrosis in the U.S., according to the Cystic Fibrosis Foundation. In people with the disease, the cystic fibrosis transmembrane conductance regulator (CFTR) gene codes for dysfunctional forms of the CFTR protein. So, when the protein does not do its job properly, it fails to move chloride – present in salt – to the surface of cells. Without chlorine, cell surfaces become dehydrated, resulting in the thick mucus lining in organs. This is why people with cystic fibrosis have a higher-than-normal level of salt in their sweat.
CFTR modulators are typically used to treat cystic fibrosis symptoms by correcting the protein. One of these includes Vertex’s Trikafta, which was approved five years ago. At present, apart from CFTR modulators in the clinic, there are other kinds of drugs being evaluated in studies as well like gene therapies.
In this article, we take a look at five biotech companies developing potentially transformative medicines to treat cystic fibrosis.
Table of contents
Enterprise Therapeutics
- Nebulized formulation of ETD001 being tested in the clinic
- FDA awards ETD001 rare pediatric disease designation
- Enterprise raises $33.1 million this year
Engrossed in lung disease therapeutics, U.K.-based Enterprise Therapeutics has created a pipeline of drugs, the most advanced being ETD001, which is being tested as a nebulized formulation – a liquid that is delivered as a fine mist to be inhaled – and a dry powder. The nebulized version of the drug is what is being evaluated to treat cystic fibrosis.
The drug works by blocking the sodium channel (ENaC) in the cells that line the lungs and other organs part of the respiratory tract. By doing so, it aims to increase hydration and clear mucus in the tract. Recently, ETD001 was awarded rare pediatric disease designation in the U.S. by the Food and Drug Administration (FDA) as cystic fibrosis is regarded as a serious or life-threatening disease. Preclinical studies revealed that low doses of the drug helped clear mucus in the airway in sheep models.
The drug candidate is currently in phase 2 studies, and the first person was dosed back in July. This trial is supported by a series B financing round that raised £26 million ($33.1 million) in January. The biotech has secured £68.8 million ($88.67 million) in total funding so far.
Krystal Biotech
- KB407: gene therapy designed to target CFTR mutations
- KB407 granted orphan drug designation by EC last year
- Krystal won $160 million in private placement last year
Immersed in the field of gene therapies, American company Krystal Biotech is working on treating numerous diseases, one of which is cystic fibrosis. The candidate KB407 is born from Krystal’s engineered replication deficient HSV-1–based platform that enables the development of gene therapies that can be administered with none to little invasion.
HSV-1 is a virus that has a large genome, and has a cargo capacity of around 30 kb – which is much more than the capacity of adeno-associated virus (AAV) vectors. KB407 is a HSV-1-based gene therapy designed to correct the mutation in cystic fibrosis by delivering two copies of the CFTR gene to the airways. The lack of functional CFTR in the airway epithelial cells results in defective ion secretion and mucus production, leading to dehydration in the airway. So, a gene therapy like KB407 can restore proper ion balance in cells and hydrate the airways in the 10% of patients who have this mutation.
The therapy was granted orphan drug designation by the European Commission and the FDA last year and in 2020, respectively.
Last year, Krystal bagged $160 million in private placement adding to its $546 million funding pot acquired over six rounds.
Recode Therapeutics
- Gene therapy RCT2100 addresses underlying cause of cystic fibrosis
- Preclinical data showed restoration of CFTR function in cells
- $250 million raised in series B round last year
Another gene therapy developer, Texas-based Recode Therapeutics is involved in making medicines for respiratory, central nervous system, and liver diseases. One of the company’s lead candidates is its cystic fibrosis gene therapy RCT2100. It is particularly for those who don’t respond well to CFTR modulators.
The inhaled drug is designed to deliver CFTR mRNA directly to target cells in the lungs, instructing them to produce a functional version of the CFTR protein. Similar to Krystal’s KB407, by providing CFTR mRNA to people who don’t have the protein, RCT2100 aims to address the underlying cause of the disease to curb symptoms.
Preclinical data showed that the gene therapy restored CFTR function in cells that were taken from people with cystic fibrosis. The drug achieved up to 135% of the efficacy seen with elexacaftor/tezacaftor/ivacaftor – a triple combination CFTR modulator – in cells with the mutation. Other studies also held up the therapy’s effectiveness after it helped clear mucus in a ferret model. The gene therapy is delivered via a lipid nanoparticle (LNP).
The first patient was dosed in a phase 1b trial in September. A year ago, the biotech snagged $260 million in a series B round, making the total money raised a total of $342 million.
Sionna Therapeutics
- SION‑638 targets NBD1 domain of CFTR protein
- SION-109: first patient dosed in January
- Sionna secured $182 million in series C financing
Set up to bring cystic fibrosis medicines to patients, Massachusetts-based Sionna Therapeutics has a pipeline of small molecules targeting the most common genetic mutation that leads to the manifestation of the disease.
With a goal of normalizing CFTR function, Sionna’s candidates target a mutation called ΔF508, which disrupts a protein that leads to the buildup of mucus in the lungs. The NBD1 domain of the CFTR protein plays a key role in the folding and stability of CFTR on the cell surface. Here, it helps regulate the flow of water as well as ions like chloride.
By stabilizing NBD1, CFTR function can be restored. This is what Sionna’s SION‑638 aims to do. The candidate received Investigational New Drug (IND) status two years ago after which it began phase 1 trials. Another one of its candidates is SION-109, which targets the interface between the intracellular loop 4 (ICL4) region and the first NBD1 of the CFTR protein. The first patient for the trial was dosed in January.
More recently, two more phase 1 trials began. In August, SION-719 and SION-451 – both targeting NBD1 – were given to patients with cystic fibrosis. The company landed a $182 million series C financing deal to further bolster its position in the cystic fibrosis space in March.
Vertex Pharmaceuticals
- Trikafta exhibits long-term benefit in patients with cystic fibrosis
- CFTR modulators phase 4 trials ongoing
- $657.3 million secured in total funding
A company headquartered in Massachusetts, Vertex is a big name in the therapeutics industry, especially in the cystic fibrosis therapeutics field. Its R&D pipeline as well as its marketed products are proof of this.
Trikafta – known as Kaftrio in Europe – which is essentially the triple-combination elexacaftor/tezacaftor/ivacaftor, has been approved by the FDA and the EC. It works by binding to different sites on CFTR proteins. Elexacaftor and tezacaftor help CFTR proteins reach the cell surface whereas ivacaftor helps these proteins stay for long at the cell surface. Long-term benefits of the drug were discovered in recent data that was presented at the North American Cystic Fibrosis Conference. The drug showed improvements in lung function in patients. Moreover, in young children, the drug boosted pancreatic function.
Vertex has four ongoing phase 4 trials and one phase 3 trial for its different combinations of CFTR modulators.
Earlier this year, the biotech’s other triple combination therapy vanzacaftor/tezacaftor/deutivacaftor was okayed by the FDA for its new drug application. It has also received validation of its Marketing Authorization Application (MAA) by the European Medicines Agency (EMA) for patients aged six years and older.
The biopharma has cashed in a total of $657.3 million in seven rounds of funding since it was founded back in 1989.
Cystic fibrosis: market on a high and so are drug prices
The global cystic fibrosis therapeutics market size was valued at $10.3 billion in 2024, and is anticipated to grow at an annual growth rate of 14.2% from 2025 to 2030, according to Grand View Research. CFTR modulators make up most of this, which have been on the rise over the past few years.
While there is no cure for the disease, gene editing offers hope to many with genetic mutations linked to the disease. In Australia, American biotech Respirion Pharma’s antibiotic RSP-1502 is being tested in patients. Since it has an efficient vibrating mesh nebulizer, it is hoped to bring down treatment time to five to 10 minutes. Furthermore, researchers at the University of Toronto found hundreds of proteins related to disease manifestation two years ago, shedding light on why some patients may respond poorly to treatment over others.
However, marketed drug prices are a concern for many, with the CFTR modulator Kaftrio costing the National Health Service in the U.K. £100,000 ($129,154.88) per person and an out-of-pocket cost of $300,000 per year in the U.S. These medicines, which have been regarded as miracle drugs, are considered out of reach by many, and there are growing calls to cut costs and involve more players in the market.
Are you interested in respiratory disease R&D?